More ER patients in Florida test positive for COVID. The surge is different this time
- Oops!Something went wrong.Please try again later.
More ER patients are testing positive for COVID in Florida compared to other parts of the country as contagious variants fuel a summer wave of infections, federal data shows.
The surge in cases is not like in previous years when hospitals were overwhelmed with patients. It’s a more modest wave, possibly boosted by people gathering during the summer, traveling and staying indoors to avoid the sweltering heat.
The most common variants circulating in the country — KP.3, KP.2, and LB.1 — have mutations that make them more contagious. And recent ER data shows an increase in sick patients testing positive for COVID at Florida emergency rooms, with levels reaching peaks not seen since the winter, according to the most recent data from the U.S. Centers for Disease Control and Prevention.

At Baptist Health, urgent care and ER doctors have seen an “uptick in COVID-19 cases in recent weeks.”
“Many patients that test positive are being treated for symptom management and not admitted to the hospital. While numbers are not comparable to that of previous surges, we remind the community to practice appropriate safety precautions,” Baptist Health told the Miami Herald in an emailed statement.
The good news is that while there’s an uptick in infections, it likely won’t lead to a surge in hospitalizations, experts say. That’s because the country has a good amount of herd immunity, either from vaccination, previous infections, or both.
About 95% of the U.S. population “currently have identifiable antibodies to omicron, specifically omicron variants, so that’s a very good herd immunity and it keeps us from having high levels of hospitalization,” said Dr. Aileen Marty, an infectious disease expert at Florida International University’s Herbert Wertheim College of Medicine. But she said the immunity “is only about 45% effective at preventing mild and moderate disease for these new strains because of those mutations that these new strains have.”
So people will get COVID, but many should be able to recover at home. Still, “a week of sort of feeling lousy and not being able to function at your optimal can really spoil a vacation in the summer,” Marty said.
As of July 5, the seven-day “moving average” of emergency room patients diagnosed with COVID in Florida has risen to 3%, putting the state just behind Hawaii for the highest percent of ER patients testing positive for the disease, CDC data show. A moving average is a way to look at trends over time by averaging data across a seven-day period. Hawaii leads the nation, with a seven-day moving average of slightly more than 4% for ER patients testing positive for COVID.
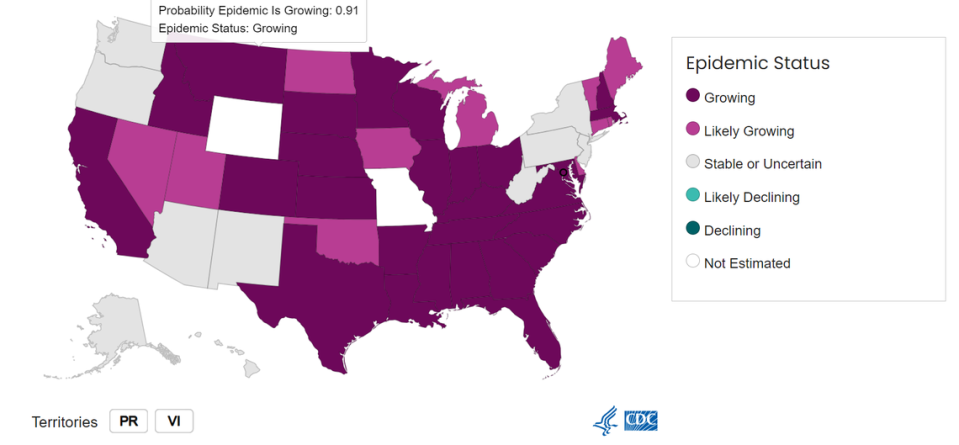
The CDC no longer tracks cases and is relying on ER visits, hospitalizations and wastewater data to gauge the COVID situation. Nationwide data shows that while COVID infections remains low, the CDC says that COVID is increasing or likely increasing across 39 states and territories, including Florida. In contrast, levels remain low in the country for influenza and respiratory syncytial virus, or RSV, a respiratory illness that causes cold-like symptoms.
Like in the past, those most at risk for severe COVID infections are 65 and older, have a pre-existing health condition or are immunocompromised.
What are the CDC’s quarantine guidelines for COVID?
CDC’s COVID quarantine guidelines have changed throughout the pandemic: If you test positive for COVID, here’s the current guidance:
If you test positive for COVID, stay home and away from others until at least 24 hours after symptoms get better overall and you no longer have fever (without the help of fever-reducing medication.)
“Depending on the length of symptoms, this period could be shorter, the same, or longer than the previous guidance for COVID-19,” the CDC states.
Once the “stay home period” is over, the CDC recommends taking additional precautions, such as wearing a mask and avoiding crowded areas for the next five days as you might still be contagious. Make sure to wash your hands frequently, too.
What COVID variants are circulating?
The dominant COVID variants in the country are KP.3 and KP.2, though scientists are also closely watching LB.1, which is picking up steam. All three descend from omicron and are offshoots of JN.1, which fueled much of the country’s winter infections.
These variants have “particular mutations that allow them to escape a lot of the immunity that the population has built up,” Marty said. They’re known as FLiRT variants based on the technical terms of their mutations, though LB.1 is also referred to as a “deFLiRT” variant because of an additional mutation.
All three variants cause similar symptoms to previous COVID strains including coughing, fever and fatigue, experts say.
While these variants are more contagious, they’re not necessarily making people more sick than other strains because of how “much immunity in the population” there is from vaccines and previous infections, according to Dr. Amesh Adalja, a senior scholar at the Johns Hopkins Center for Health Security. His work is focused on emerging infectious disease, pandemic preparedness and biosecurity.
Other things to know about COVID variants:
▪ The most dominants variants in the country are KP.3 and KP.2, which are estimated to make up about 25% and 22% of the country’s cases, respectively, according to the CDC’s most recent estimates. LB.1 makes up about 10% of cases.
▪ In the region that includes Florida and seven other states in the southeast, the variant rankings are flipped. KP.2 is slightly ahead of KP.3, and is estimated to make up nearly 35% of the cases, CDC data shows. KP.3 makes up nearly 31% of cases. Both JN.1 and LB.1 each make up nearly 6% of cases.
READ MORE: COVID infections are on the rise in Florida. What to know as new variants circulate
Are COVID vaccines still effective?
While COVID vaccines should still provide some protection against the virus, enough to reduce the risk of severe illness, studies show that the existing shots appear to be less effective against the circulating variants.
“For high-risk individuals, the vaccine is still life-saving,” said Adalja, the Johns Hopkins expert.
Updated vaccines are expected to roll out in the fall.
This time, the FDA wants the new shots to better match JN.1 and its descendants, like KP.2 and KP.3. The goal is to update COVID vaccines annually, similar to flu shots, to boost protection.
“When these vaccines first became available [in 2020], we were still in the midst of having seen just a tremendous amount of severe disease and deaths from COVID-19,” said Marty, the FIU expert. “We didn’t have the antivirals like Paxlovid that we have now ... people did not want to end up in the hospital and that drives people to get vaccines a lot more than, ‘Oh, well, I might get a lousy cold.’”
After the first sought-after COVID shots were rolled out, people’s interest in receiving updated vaccines has steadily dropped, despite federal outreach efforts. People are still dying from COVID, but it’s not like the first waves of the crisis. COVID is no longer a pandemic and is more endemic, which means the disease is circulating but is not out of control.
“When the ancestral strain came out killing people, you couldn’t call your doctor and ask for Paxlovid. It didn’t exist,” Adalja said. Doctors now know how to treat the disease. And people have some immunity against COVID, either through vaccination, a previous infection, or both.
But because the virus that causes COVID is constantly mutating, people’s immunity declines over time. Just like flu vaccines, COVID vaccines are meant to help bolster protection, experts say. But getting people to roll up their sleeves for a shot has been a challenge.
Vaccinations remain low nationwide with about 21% of adults and 14% of children estimated to have received the updated 2023-2024 vaccine, which was released last fall, according to the CDC.
In Florida, about 16% of adults and about 9% of kids have received the updated shot, as of the CDC’s most recent update in May. In comparison, about 70% of adults in Florida had completed the primary two-dose COVID vaccine series, as the Miami Herald has previously reported.
There’s no one reason why people have passed on the new vaccines — the politicization of the shots, concerns over side effects, misinformation, and a person’s lack of concern over their COVID risk are some of the reasons some might avoid the shot.
READ NEXT: Fewer in Florida are getting new COVID shot. Why they’re refusing — and what it means
In this new era of COVID, public health experts are encouraging people to consider their risk factors for severe illness. Some of those most at risk for severe disease include people who are pregnant, at least 65, immunocompromised or have a pre-existing health condition such as obesity, diabetes and kidney disease. Young kids who have never been vaccinated are also at risk, experts say.
“The reason to get vaccinated is not, in this current era, is not to prevent yourself from getting infected,” Adalja said.
“It’s to prevent yourself from getting severe disease,” he said, noting that even the currently available vaccine is “highly effective at prevention of severe disease, hospitalization and death, which is what we want the vaccine to do.”

