In the Next Wave of Cancer Research, Anybody Anywhere Will Be Able to Help
Nikhil Wagle, a medical oncologist, studies the genetics of tumors at Dana-Farber Cancer Institute and the Broad Institute. Both are major centers for cancer research and treatment, and both are located in the greater Boston area. While the work is invaluable, not everyone has access to a major city or cancer research center. Wagle said his colleagues came to wonder, "How much more progress could we make if anyone could contribute their samples and their data for research?”
This insight led to the creation in 2015 of the metastatic breast cancer project, which uses social media and other technological advances to allow patients, even those far from a cancer center, to share their medical information and tissue, blood, and saliva samples with researchers. Three similar projects were subsequently launched to target different cancers, [1] and in 2018, Dana-Farber and the Broad partnered with the Biden Cancer Initiative and the Emerson Collective [2] to launch a non-profit called Count Me In.
Wagle and his colleague Corrie Painter, a biochemist and expert in cancer immunology, together direct Count Me In. They talked to Popular Mechanics about the organization and the emerging model of patient-partnered medicine that it exemplifies-including how the program works, the progress it’s made, and the risks and benefits of bringing what is essentially a crowdsourcing model to medicine.
This interview has been edited and condensed.
What are the actual mechanics of Count Me In? If I’m a patient who wants to participate, what does that actually look like?
Corrie Painter: A patient joins by finding a URL online for any of our projects. So for example, our first project, the metastatic breast cancer project, can be found at mbcproject.org. On the home page it describes what it is we’re doing. Anyone who wants to participate can click on the “Count Me In” button, and that takes them through an online survey, as well as an informed consent process. If they opt in to join the study, we ask the fewest amount of questions possible to understand who is signing up, to make sure they have the cancer we’re studying. After they complete that-which for the metastatic breast cancer project takes 6-15 minutes total-that triggers our internal processes. We send them a saliva kit and in some cases a blood biopsy kit. That gets shipped to their house. These kits have instructions in them; they have self-addressed pre-stamped envelopes. And then everything else is kind of up to us. And part of that is communicating back what it is we’re learning as often as we can. We make figures and graphs to show who is participating. We present at scientific conferences. We’ll do lay walkthroughs and make videos of those and send them through to patients so they can have a sense of where we are, with respect to the research that they’re participating in. And then we deposit that data into the public domain so other researchers can access it and make discoveries.

Is this a new approach?
Nik Wagle: The concept of partnering with patients is not a brand-new idea; there are examples even in cancer research that go back many, many years. And then if you go to other diseases, particularly rare diseases, there are examples of these patient partnerships. But in the past, the way to do this was really different and much harder. There were letter-writing campaigns and advocacy groups. And the opportunity to scale or to do something like this in multiple cancer types across multiple regions was really hard. We were inspired by projects that came before us, but really wanted to take this to the next level by incorporating social media, and the Internet, and form advocacy groups, and engage families. [3]
What is the level of engagement? Participants are people with a personal stake in this, but my cynical expectation would be that this is like checking the organ donor box, where patients don’t want to do any work. Where they say, I feel good about contributing to the research, but I don’t need to watch all the talks.
Wagle: Many of the patients in our projects don’t have cures. So participation is really different than checking a box and saying, I’m an organ donor, which is different and removed. These are patients who are facing these diseases every single day, and want to be empowered to be able to do something.
Painter: There’s definitely people really keenly interested in every step along the way, and then there are people who just, overwhelmingly, want to know that it matters. When I think back through the catalogue of experiences with so many patients, there’s one that sticks out. We were previewing the data for the first release with the metastatic breast cancer project, and I showed this to one of our patients that was very involved with the build of the project and the beta testing. This was just several weeks before she passed away, and we wanted to make sure she was the first patient to see that data. We walked her through it and she looked at the magnitude of the data without really knowing what any of it represented. And she just took pause, and she said, “Oh my God. I’m not alone.”
Do these projects go back to patients to get updated clinical information, or to have them do additional questionnaires as studies progress?
Wagle: We do. We have a bunch of information, surveys, medical records, samples that we collect at the beginning. But we have serial surveys. We can go back and collect additional blood samples or additional tumor samples or updates to the medical records. But also, let’s say we make a discovery and it turns out there is a particular subset of patients for whom there is some interesting finding that we discover based on looking at the genomic sequences in their tumor samples. We can then go back and send a targeted survey or request for something additional from that subgroup.
Do you see a lot of attrition-cases where the patient chooses not to participate moving forward?
Painter: It’s really difficult to answer that. We don’t know how many patients are still alive at the time that we may do follow up. But you can estimate based on the average expected lifespan of somebody. For example, with metastatic breast cancer it’s three years, so if we put a survey out at the three year mark, certainly not everybody who signed up in the first place will still be alive to take that survey. So that being said, to our great surprise, we recently put out a survey in that project and I think within the first week had over 800 people fill that survey out, and 1,350 total, which is a huge number of people that we can continue to learn from. We have another signal along this line, which is the fact that we have over 1,000 blood biopsies-which is part of the project we added several years after we launched. [4]
It seems like a big advantage to this approach is that as technology develops-maybe there’s some new gene sequencing technology, or something that arises after I’ve sent in my tissues, or even when I’m no longer alive-Count Me In can still put my tissues through those kinds of tests. I can still contribute. Are there technologies that have developed since you started the project that now patients are ‘getting access to,’ that they wouldn’t have otherwise?
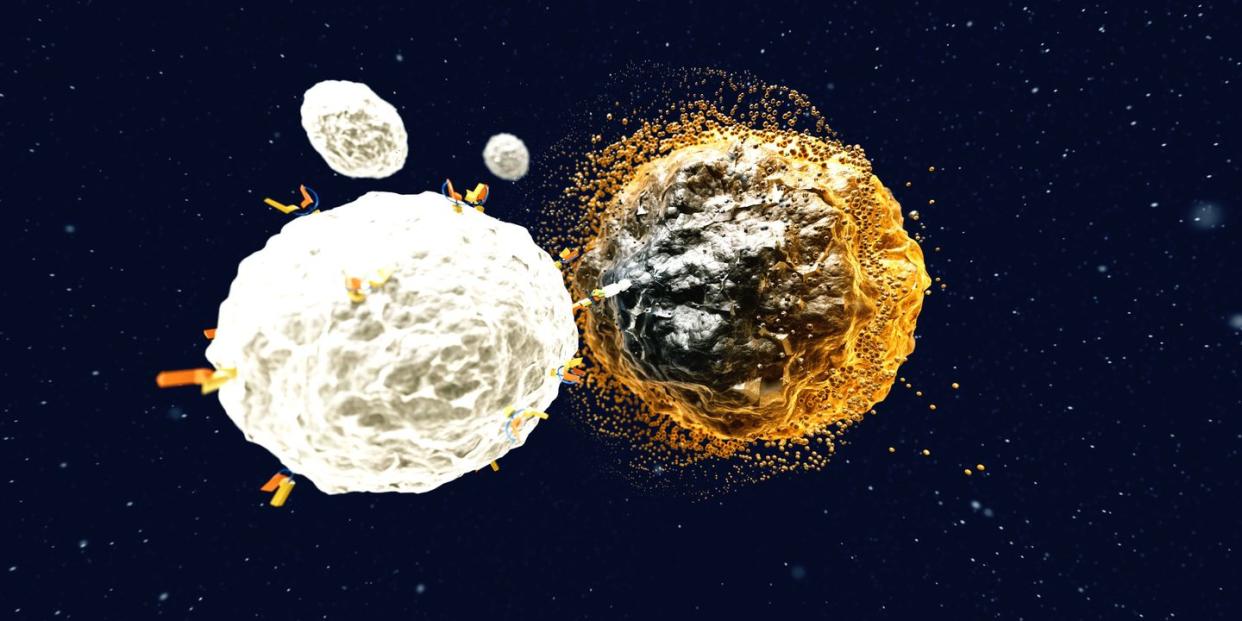
Wagle: The point that Corrie just brought up, about the blood samples-when we first started the MBC project in 2015, the technology to sequence tumor-derived DNA that’s circulated in the blood was not quite as robust as it is now. So we always had the idea that we might someday collect blood samples from patients, so we could view what’s called a liquid biopsy-basically, to look at their tumor just from a tube of blood. And that technology developed and matured over the course of the first couple years of the project. There are other technologies that allow us to do really detailed analysis of proteins at the single-cell level from tissue slides that didn’t exist in the same way when we started this project. So now we’re getting tumor samples from patients, we’re getting a few extra slides to try to be able to use these new technologies. [5] Anytime patients participate, they’re really leaving a legacy to be able to contribute to research both now and in the future.
That brings up an interesting point, which is that you’re collecting and tracking lots of data about these people-and that kind of thing can really freak people out. What is the level of comfort you’ve seen in patients? What are the fears people have?
Wagle: One observation: The patients who are electing to participate in these studies, they’re saying, Count Me In. I’d like my information and my samples to be shared with the research community to try to accelerate progress and make advances in finding new treatments for my cancer. A lot of times what we hear is, I know this may not help me, but if it can’t help me, maybe it’ll help the next person, or my kids, or somebody who may get this disease in the future. As long as they trust that we are going to do everything in a way that protects them and protects their confidentiality and protects their security, which we do. We have the same type of security information systems that protect people’s confidentiality in hospitals. [6] We use all the standard security measures to keep people’s information de-identified, and when we share the data, we strip everything of readily identifiable information. But patients are told: we’re not doing this in a way that’s limiting. We’re trying to break the mold-all this data is usually kept locked up in silos; we’re trying to unlock the data and share it.

Aside from security, there is another concern. The trite saying is, if the service is free, that means you’re the product. [7] There was recently a series of scandals at Memorial Sloan Kettering, a major cancer hospital, and one of them was about research being turned into a product without patients’ knowledge. [8] Do you think about whether this work could lead to an ethical quandary at some point-say, if people turn over their information and then a very lucrative treatment regime comes out of it?
Wagle: We think about it all the time. One of our first and most important core principles that we tell everyone-it’s in our consent form-is that we will never sell your data. The partnership is: you share your data, we generate genomic data and aggregate it, and then we make it freely and publicly available without restriction on a regular, ongoing basis to anyone who wants to use it. So I think it’s really different than the Facebook example of, if it’s free, then you’re the product. The other example you alluded to, which is where people are taking medical data without consent and monetizing it-we take that really seriously. We do nothing without explicit consent to use the data in the way we’re going to use it. If then people take freely available data and make a drug, and make a ton of money with it, [9] everyone should be really happy that their contribution led to a drug that’s going to help a lot of people.
Painter: At the end of the day, if this data isn’t leveraged to make better drugs and clinical trials that save people’s lives, then I’m not really sure what the point is.
So where does this organization go from here? Are there other diseases besides cancer that this approach would be particularly fruitful for?
Wagle: As we continue to sequence samples in the two most mature projects-the angiosarcoma and the metastatic breast cancer projects-we continue to make discoveries. There’s data out in the world, and we recently learned that there are now a number of publications that have used that data in their own studies, [10] so this data is being used in the exact way we intended it to, which is that the research community is taking to it and using it without having to call us up and say, can we please work together? Our goal is over the next several years to launch projects for every major cancer type as well as rare and pediatric cancers. So that’s the road map. And we are focused on cancer because that’s our background, and there’s a lot of work that needs to be done in cancer. But I think if this approach starts to scale beyond cancer that would be great, too-but that’s probably for the future.
[1] Currently, Count Me In consists of four projects: metastatic breast cancer, angiosarcoma, metastatic prostate cancer, and esophageal and stomach cancer. Brain cancer and osteosarcoma projects are in development.^
[2] Emerson Collective is an organization founded by Laurene Powell Jobs to back initiatives to effect change on a wide variety of issues, like immigration, the environment, and healthcare. Powell Jobs is the widow of Steve Jobs, who died in 2011 from complications from liver cancer; he famously spent months after his diagnosis pursuing alternative treatments, possibly to his detriment. Their son, Reed, is the director of Emerson Collective’s health practice. ^
[3] Another major project in this mold, the National Institute of Health’s “All of Us” project-also launched in 2018-uses a similar protocol with a much broader ambit: its goal is to enroll more than 1,000,000 participants and study a wide variety of diseases. ^
[4] As of this writing, 6,500 people have submitted their information, and Count Me In has more than 4,600 saliva, blood, and tissue samples. ^
[5] Count Me In-affiliated projects store minimal amounts of biological material. For tissue samples, like tumor biopsies, they only take as much as they need for their tests, then return the rest to the patients’ hospital. ^
[6] Rules around privacy of health information largely come from the Health Insurance Portability and Accountability Act of 1996 (HIPAA). You can read more here. ^
[7] This saying has in recent years been repeatedly deployed to call attention to the fact that many digital services are free to users only because the business model is not to sell the service, but to sell the users’ data. Interestingly, it traces its origins much further back than the inception online advertising. ^
[8] Sloan Kettering was wracked by a series of scandals uncovered by reporting by ProPublica and The New York Times. One involved an AI startup that was given exclusive access to an archive of patient tissue slides. A report notes, “Hospital pathologists have strongly objected to the Paige.AI deal, saying it is unfair that the founders received equity stakes in a company that relies on the pathologists’ expertise and work amassed over 60 years. They also questioned the use of patients’ data - even if it is anonymous - without their knowledge in a profit-driven venture.” ^
[9] NB, Count Me In is a nonprofit organization. ^
[10] According to Count Me In, at least nine groups have published studies using the organization's data. One sample finding: the genetic pathways to angiosarcoma are similar in humans and dogs. While that may seem like a completely useless thing to know, it's not. As the authors of that study note, angiosarcoma in humans is "both rare and heterogenous, making large, well powered genomic studies nearly impossible." In dogs, however, it's quite common; if the genetic pathways are similar, dogs could potentially be used as a model organism for pushing forward with study beneficial to human patients. In other words-and somewhat poetically-the finding is important because there are enough dogs with angiosarcoma to do the kinds of research that CMI is working to make it possible to do in humans. ^
('You Might Also Like',)

