NJ COVID hospitalizations still spiking, but patients recovering faster than in first wave
- Oops!Something went wrong.Please try again later.
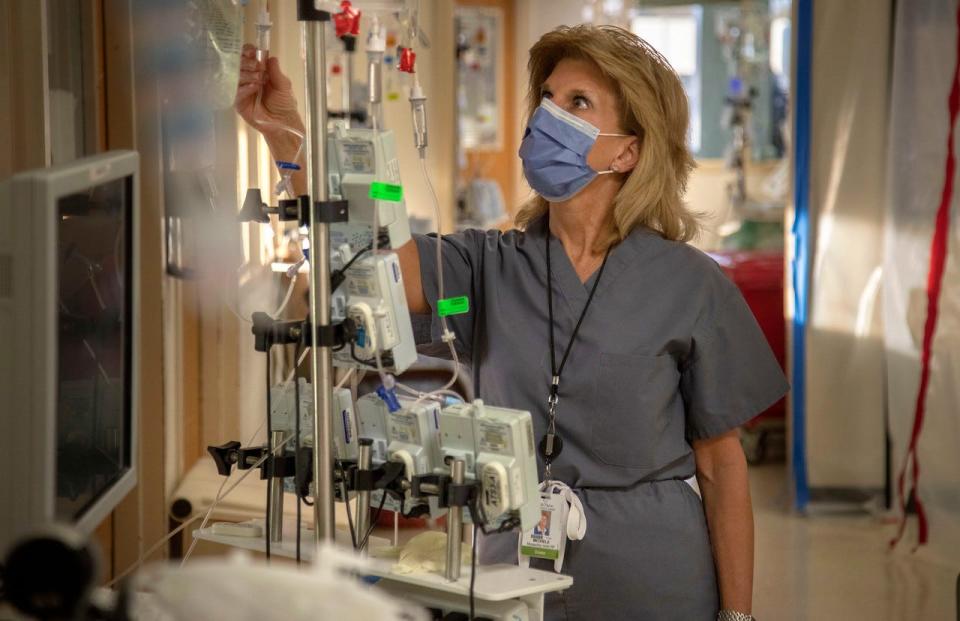
For COVID patients who are hospitalized, this wave of the pandemic — the omicron wave — is different.
They are likely to spend less time in the hospital — five to eight days, compared with 10 to 15 in previous surges.
They are less likely to need intensive care or a ventilator. High-flow oxygen to aid breathing is more common, while ventilator use has shrunk to a third or less of ICU patients.
And the vast majority recover. This time around, there are no morgue freezer trucks.
The surge in COVID patients in New Jersey hospitals hit 5,155 on Tuesday, a high not seen since May of 2020. It is expected to peak in mid-January at numbers that could exceed the pandemic’s devastating first wave. Health officials warn of unprecedented staff shortages.
“The only silver lining in this is that the patients are not as sick,” said Dr. Robert Brenner, president for clinical integration and physician enterprise at Valley Health System, where in the last six weeks the number of COVID patients spiked from three to 122. “They’re coming in quicker, getting sick quicker, getting better quicker and going home.”
Hospitals are operating differently, too. They haven't needed to reopen the hastily created overflow COVID units of 2020. They can accommodate their census of COVID patients in regular hospital wards, albeit carefully segregated from other patients.
Most importantly, they can continue to care for patients who don’t have COVID.
That includes stroke and heart attack patients whose avoidance of medical care in 2020 led to higher mortality rates statewide, and gunshot and accident victims whose numbers haven’t dipped, since businesses and social gatherings are not locked down as they were during the pandemic's first wave. In fact, at St. Joseph’s Health in Paterson, a big concern is the shortage of blood for trauma patients.
But while that’s mostly good news, hospital officials say they’ve never seen so many employees out sick.
Health Commissioner Judy Persichilli this week told health care executives to prepare for staff absences as high as 30%. But some facilities are already nearly there — and the omicron spike hasn’t peaked yet.
“This is something we’ve never seen before, the rate of contagion with omicron,” said Michele Acito, executive vice president of Holy Name Medical Center in Teaneck. “We have more than 100 employees who are out.” Holiday gatherings and community spread have driven the infections, not in-hospital transmission, executives say.
Story continues after chart
Hospital staff absences are at the highest levels reported during the pandemic — there were 574 new infections confirmed on Monday, with 302, 462 and 727 each day before that — compared with 107 a year ago.
Limited staffing combined with huge numbers of patients seeking emergency care have led some hospitals to divert ambulances from their ERs. On Tuesday afternoon, 10 hospitals were on full or partial divert.
All of them have a plea: If you need a COVID test, go to a testing center, not the hospital emergency department.

At St. Joseph’s Health, 60 employees could not work on Monday because they tested positive, while only 16 were able to return to work after quarantine or isolation, said Dr. Joseph Duffy, the chief medical officer. “My concern is the gap is widening,” he said.
The cut in quarantine time recommended by the federal Centers for Disease Control and Prevention after exposure to COVID has helped. Following a change in the guidelines last week, those who are asymptomatic need to stay home for only five days, down from 10.
“It's made a significant difference,” Acito said. “Ten days was putting us in a difficult position.” Employees returning to work are feeling well-supplied with enough personal protective equipment to keep them safe — and they are needed, she said: “We have a lot of work to do here.”
But most hospital systems have been forced to reassign staff to fill the vacancies. Operating room nurses and those who usually do post-anesthesia care are now working on medical/surgical floors.
“People have stepped up to take on new roles as needs change," said Brenner, of Valley Health. They “have shown an incredible strength in dealing with a very difficult situation to ensure that patient care is not impacted.”
Contingency staffing
St. Joseph’s two hospitals, in Paterson and Wayne, have moved to “contingency staffing” — a step down from business as usual, and not yet as dire as crisis standards, Duffy said. “We do have a crisis-level plan ready to go,” he added.
Crisis standards mean that “you totally change the way you take care of patients,” Persichilli said. In a crisis period, a team makes rounds once a day to take care of “necessary and immediate needs” of up to 15 patients. The most highly skilled workers are saved for tasks that only they can perform, such as wound care or medication administration, while less highly trained employees fill in behind with tasks such as patient repositioning and hygiene.
Story continues below chart
St. Joseph’s went to contingency staffing on Dec. 24, “when we saw a staffing crisis … and immediately canceled all Level 4 and Level 5 surgeries,” Duffy said, referring to cosmetic and other procedures that can be postponed without negative health consequences. As of Tuesday, “95% of Level 3 surgeries have also been eliminated,” he said. Those procedures, for which delays may affect the health of the patient, are decided on a case-by-case basis, he said.
Some patients with upcoming procedures scheduled at Hackensack Meridian Health hospitals are being told to postpone their appointments, too. "We want to make sure we can get people in who have medically necessary, time-sensitive procedures and get them taken care of," said Dr. Daniel Varga, the system's chief physician executive.
Delays for the others probably will extend to late January and early February, he said. "We're not kicking these out 60 to 90 days."
Other hospitals in New Jersey may follow contingency standards soon, said Cathy Bennett, president and CEO of the state hospital association.
The state has applied to the Federal Emergency Management Agency for strike teams totaling 150 personnel to assist hospitals, said state police Superintendent Patrick Callahan, who heads the state Office of Emergency Management.
Most COVID patients are unvaccinated
Despite more breakthrough cases, unvaccinated patients still make up the majority of COVID hospitalizations, according to data from the New Jersey Hospital Association. A survey of patients on Dec. 31 showed that 60.6% were unvaccinated.
Another 33.6% were "under-vaccinated," meaning they either received only one shot of the Pfizer or Moderna vaccine or have not received a booster shot. And 5.8% were fully vaccinated plus a booster shot.
Those who are severely ill tend to be elderly or have the same underlying medical conditions that led people to need hospital care earlier in the pandemic — obesity, diabetes and high blood pressure, hospital executives said.
The vaccinated and boosted don't get as sick. They “are going to get treated and go home,” generally without complications, said Acito, of Holy Name. “It’s the unvaccinated who often are ending up in the ICU.”
Compared with earlier waves, a smaller percentage need intensive care. At Hackensack Meridian Health's hospitals, 140 of 1,100 COVID patients on Tuesday, or 13%, were in ICUs, and 75 were on ventilators. That's down from about 20% requiring ICU care at the pandemic's start.
Some patients are admitted for other illnesses, only to discover after admission testing that they have COVID. Over the last month, that portion has increased to “45% who were admitted for something else but were found to have COVID, too,” Bennett said.
While most health experts assume that the spike in cases is driven by the omicron variant, last week the majority of COVID patients hospitalized at Hackensack Meridian Health hospitals actually had the delta variant, said David Perlin, the system’s chief scientific officer. That is likely because the system performs variant analyses only for its hospitalized patients, who clearly have more severe disease than the general population with COVID.
Other hospitals send a sampling of their patients' COVID test specimens to the state Department of Health laboratory, which does not tell them which variant has been detected.
The COVID treatment available has also changed since the pandemic's early days. Monoclonal antibodies that were effective against previous variants are no longer used for patients presumed to be infected with omicron. But the one antibody treatment considered effective is in short supply, and its use is strictly limited to those who meet the CDC’s criteria.
Lindy Washburn is a senior health care reporter for NorthJersey.com. Scott Fallon contributed to this story. To keep up-to-date about how changes in health care affect you and your family, please subscribe or activate your digital account today.
Email: washburn@northjersey.com
Twitter: @lindywa
This article originally appeared on NorthJersey.com: NJ COVID hospitalizations still rising, patients recover faster

