A new non-surgical procedure is helping those with emphysema breathe better. The only problem? Not enough people know about it.
MILWAUKEE — About two years ago, John McLees' lungs had become so badly damaged that he could barely get from one side of his small condo to the other without feeling like he'd just finished an intense workout.
McLees, of Germantown, was born with a genetic condition called Alpha-1 Antitrypsin Deficiency, which increases his risk of developing lung and liver disease.
As he aged, the condition ravaged those organs. In 1999, he got a liver transplant, which stopped the mounting damage.
But the transplant couldn't reverse 60 years of damage already done. He was well on the path to developing severe emphysema, a disease that ruins the wall structures of the lungs, making it so air gets trapped inside and they overfill.
McLees went from only having to wear an oxygen tube at night to having to wear it 24 hours a day. He struggled to walk short distances, much less exercise. His sedentary lifestyle further worsened his health and his relationships.
Related video: Fate and TV news unite grieving parents and a heart transplant recipient
He felt like a burden, avoiding birthday parties for many of his 36 grandchildren. He missed baseball games and school concerts, he said, feeling like having him around was a "pain in the neck" to his loved ones. He even attended church from home, watching alone on TV. McLees' wife had died decades ago, shortly after his liver transplant, making it even more isolating.
"I've always been a very positive thinking person. So, I didn't let it drag me into a depression," he said. "And the kids stopped by, but even them stopping by and little ones coming into the house, I wasn't able to participate. You know, I'd sit there and watch."
Several years ago, patients like McLees would have had few options. If inhalers, oxygen pumps and pulmonary rehab stopped working, the only options left were major surgery: a lung transplant or lung volume reduction surgery, which removes damaged portions of the lungs.
OMICRON BOOSTER: FDA authorizes reformulated COVID-19 booster shot for the fall

Instead, about 18 months ago, McLees' doctors at Froedtert and the Medical College of Wisconsin presented him with a middle option — one that wouldn't require a single cut, and could easily be reversed if it didn't work.
By placing tiny, one-way valves in the air passages that lead to the most damaged parts of his lungs, doctors could essentially take an entire section offline to allow the healthier parts of his lungs work better.
The valves, which expand to fit right in the passageways, only let air out, not in, causing the damaged section to deflate and not fill again.
"It's less invasive, and it can have just an incredible impact," Dr. Jonathan Kurman, an interventional pulmonologist with the Froedtert and MCW health network, said of the procedure, called bronchoscopic lung volume reduction.
For the patients for whom the procedure works, many of whom are of older age, the valves can bring a chance to return to who they were perhaps a decade earlier, before chronic lung disease kept them from being able to walk through a grocery store or make it upstairs to their bedroom.
"It's stuff that a lot of us take for granted, but when you can't do it, it really impacts your life," Kurman said.
It didn't take too much explaining for McLees, now 80, to decide that "all signals were go."
"When you get down to a point when you can't walk 30 feet without losing your breath, if someone throws an inner tube at you, you're going to grab it," he said.
MORE: Millennials and Gen Z more likely to develop hypertension, preeclampsia while pregnant, study shows

'A lot of it is patient initiated'
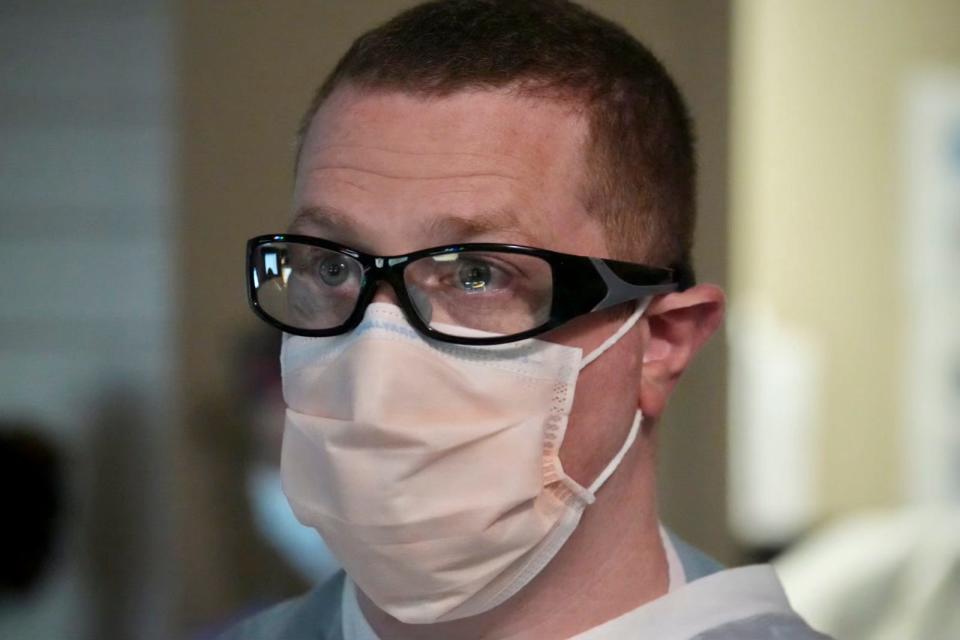
In a dimly lit procedure suite on Froedtert Hospital's campus, Kurman peered through safety glasses at a TV screen as he clutched several tubes that were coming out of his patient's mouth.
The patient, 78-year-old Roger Rose, was sedated. Kurman's first task was to snake a camera down Rose's windpipe and into the intricately branched airways of his lungs, to scope out the best spot for the valves.
Overall, most of the valve procedures only take about a half hour, and don't even require a sterile surgery suite. The average person gets four to six valves, which expand and sit in the airways without any stitches or cuts.
Patients stay in the hospital for a couple of days after the procedure for observation. Then they're released and monitored. If for any reason the valves don't work, they can be easily removed in minutes, Kurman said.
According to data from Pulmonx, which created the valves, some 25,000 patients around the world have received the procedure. The U.S. Food and Drug Administration approved the technology in 2018, and there are 250 hospitals using Pulmonx's valves in the U.S., including five in Wisconsin.
Froedtert Hospital, under Kurman's leadership, was one of the first in the state to start offering the procedure. The health system has completed the most valve procedures in the state — nearly 100 since they started in November 2019 — and also ranks third in the Midwest and eighth in the country for how many times the procedure has been performed.
The procedure is covered by most insurances; Kurman has never had a situation where insurance providers did not cover a patient who qualified. Despite that, and even though the valves have been used in Europe for about 15 years, the procedure is relatively a "newborn" in the U.S, Kurman said.
To Kurman's surprise, the lack of awareness among other doctors about the valves has led to many patients coming to his office after doing their own research and self-advocacy. Many learn about the valves online or on social media, in several cases through a 5,400-member-strong Facebook group called "Lung Valves For Friends."
"A lot of it is patient initiated, and it's different from everything else that I do in that sense," Kurman said. "Everything else is doctor-driven."
He wants more doctors and patients to know it's an option, he said.
"So many of (my patients say), 'I wish I had heard about this a couple of years ago,' or 'How come no one's talked about this before?'" he said. "So, one of my big initiatives is just to try to increase awareness among patients and providers that this is available. It's not a trial anymore. It's not experimental anymore. It is very safe."
In Rose's case, the valves were successfully placed to deflate the entire upper left lobe of his lung. In effect, Kurman told his team, he'd performed a lobectomy, a major surgery in which a whole lobe of a lung is removed. But in this case, it was all done without a single cut.

'A phenomenal change in my life'
More than 3 million people in the U.S. have emphysema, according to the American Lung Association. While there are other causes of emphysema, like McLees' genetic condition, the No. 1 cause for the disease is smoking, and because of that, it is considered to be highly preventable.
Procedures like bronchoscopic lung volume reduction are part of a larger push in medicine toward less invasive treatments. The procedure gives patients who've spent years struggling with lung disease an option between medicines and major surgery.
"When you need surgical intervention, you need it," Kurman said. "But if you can accomplish the same thing or something very close without surgery, I think that that's the appropriate way to start."
For McLees, the relative improvement has given him a bit of his life back.
He still has to wear an oxygen tube but is down to a 3-liter tank instead of a 5-liter one. Sometimes, he can pull the tube off while he makes a stop at the supermarket to quickly grab something he needs. He can be present and active around his kids and grandkids. He can hold a phone conversation for more than 30 seconds.
"It's been a phenomenal change in my life," he said.
Follow Devi Shastri on Twitter at @DeviShastri.
This article originally appeared on Milwaukee Journal Sentinel: New lung valve procedure helps emphysema patients avoid major surgery

