Not just fentanyl. Animal tranquilizer xylazine is embedded in Ohio's drug supply
A Northern Kentucky doctor saw a patient who was hospitalized for weeks as caregivers removed all the skin from her forearms to save them from amputation.
Dr. Mike Kalfas said the woman had been using the opioid drug fentanyl tainted with an animal sedative that caused tissue death, a situation that's becoming more and more common in the Cincinnati area.
“I’ve been educating my patients,” Kalfas said. “I’ve been telling them, look, there’s some bad stuff that may be in your drugs that Narcan won’t save you from.”
That stuff is xylazine, often called tranq dope, and it’s the newest challenge in the opioid epidemic. The drug is cheap and easy to get, so sellers add it to their fentanyl supplies to multiply their profits. It lengthens the euphoria effects for people who use drugs but causes chaotic health conditions.
Xylazine started appearing in the northeastern United States several years ago but exploded around 2020, with Philadelphia as the hub. And while some amount of xylazine has been found in nearly every state, the hot spots are spreading west. Ohio, Indiana and Kentucky are besieged. The trend is following the same path fentanyl did a decade ago.
"It's called tranq,” said AmandaLynn Reese, chief program officer for Harm Reduction Ohio. “We call it tranq because it is one. It's a tranquilizer that's used for livestock."
Columbus seeing increase in xylazine cases
Since a change in Ohio law in late March that made xylazine a controlled substance, police have started tracking the number of cases.
Columbus police said xylazine had been found in combination with fentanyl or fentanyl-related substances for several years, Columbus police public relations specialist Andres Antequerra said. However, because the drug was legal until March 29, 2023, it wasn't tracked as an illegal narcotic until this year.
As of Monday, Columbus police's crime laboratory had reported xylazine 72 times. All but four of those instances have involved xylazine being found in combination with fentanyl or a fentanyl-related substance.
The Franklin County Coroner's office does not currently track deaths related specifically to xylazine, however, the number of presumptive overdose deaths as a result of fentanyl overdose were slightly higher through the first half of 2023 when compared to the first six months of 2022.

The Cincinnati area is a trouble spot for ‘tranq’
As addiction doctors, harm reduction workers, public health and crime lab officials witness the manifestation of xylazine in the Cincinnati area, experts watching xylazine’s part in the opioid crisis caution there aren’t enough tests across the country to understand its impact.
In September, a San Diego-based drug testing laboratory called Millennium Health issued a report showing the drug’s prevalence in drug tests that doctors ordered throughout the United States.
The researchers looked for xylazine in more than 160,000 fentanyl-positive specimens starting April 12, the day the White House issued a nationwide warning about the drug, and ending July 20. Then they ranked states with the most xylazine-positive tests. Ohio, Indiana and Kentucky ranked Nos. 3, 5 and 7, respectively.
Dr. Roberto Soria, CEO and medical director of the Crossroads Center, a methadone and addiction clinic in Corryville, suspected xylazine was causing complications for some of his patients and first ordered tests for the drug in April.
He said the analyses showed 1 in 4 of the tests that were positive for fentanyl were also positive for xylazine. He followed these results, averaging more than 500 tests each month. In September, he said the ratio jumped to more than 1 in 2.
The Hamilton County Coroner and Crime Lab also reported a jump in xylazine-positive items from 1,541 in 2022 to 1,594 from Jan. 1 to Sept. 30. The same office saw a jump in xylazine’s presence in overdose deaths, from 48 between April and December of 2022 to 86 between January and September of this year.
“It’s another evolution of this fentanyl crisis,” said Eric Dawson, vice president of clinical affairs at Millennium Health, and an author of the report.
Tranq dope: Animal sedative xylazine made a controlled drug in Ohio

‘Horrifying’ health threats follow animal sedative xylazine
Health threats from xylazine are sweeping, from a slowing heart rate, low blood pressure and amnesia to devastating skin damage. A person can ingest the drug without knowing it, leading to an agonizing withdrawal that may prompt people to recoil from getting medical care.
Dr. Richard Ryan, an emergency medicine physician at the University of Cincinnati Medical Center, said his department is seeing an uptick of patients suffering from xylazine-related health crises.
“Don’t assume it’s safe,” he said. “Inhaling it, ingesting it, does not prevent you from getting the complications.”
The drug is often used to sedate cattle, sheep, horses or dogs, and is “very complicated,” Ryan said, as it attacks the body in multiple ways.
Xylazine decreases adrenaline, he said, causing sedation. That drop may lead to a dangerously slow heart rate, low blood pressure, respiratory depression and more. It can also narrow the microscopic arteries in the skin, decreasing blood supply to the skin and creating open sores, which can become gaping wounds.
The sores may appear anywhere on the body, according to medical articles. Unlike injection sores that intravenous drug users may suffer from, xylazine wounds are a systemic effect of the drug itself. And as the open wounds progress, the tissue affected can die.
Brandi McNamee, a nurse for the Butler County General Health District, has noticed more clients with xylazine sores at the county’s safer drug-use sites. She offers to clean the wounds, and the site provides wound care supplies.
But sometimes skin around a wound is “hard and black,” she said. It's dead tissue. When McNamee sees that, she urges the client to go to a hospital. Doctors have to remove all of the dead skin.
Soria, too, said he's seeing “a significant increase” in skin wounds and mixed fentanyl and xylazine withdrawal. “This makes it that much more difficult for my patients to stop using illicit street opiates,” he said.
Withdrawal from the animal sedative is harrowing, Ryan said. Sufferers experience high levels of anxiety, a rapid heart rate, and high blood pressure, among other symptoms.
One of the biggest problems, as xylazine sweeps the country, is its under-recognition, said Dr. Kelly Ramsey, chief of medical services for the New York State Office of Addiction Services and Support.
People may not know they’ve used xylazine. Medical examiners don’t always test for it, and crime labs often don't have the tools. “We lack best practices to treat xylazine wounds, treat xylazine withdrawal, and manage xylazine use disorder,” Ramsey said.
A xylazine overdose is harder to reverse because it does not react to naloxone, and bystanders who try to revive someone might not realize what’s going on. Ryan said people still should use naloxone if they see someone who appears to be overdosing. They have often ingested fentanyl, too.
If that doesn’t work, “call 911,” Ryan said. “Start CPR.”
What is xylazine? What you need to know if someone you know uses fentanyl

Xylazine test strips are available, but often illegal
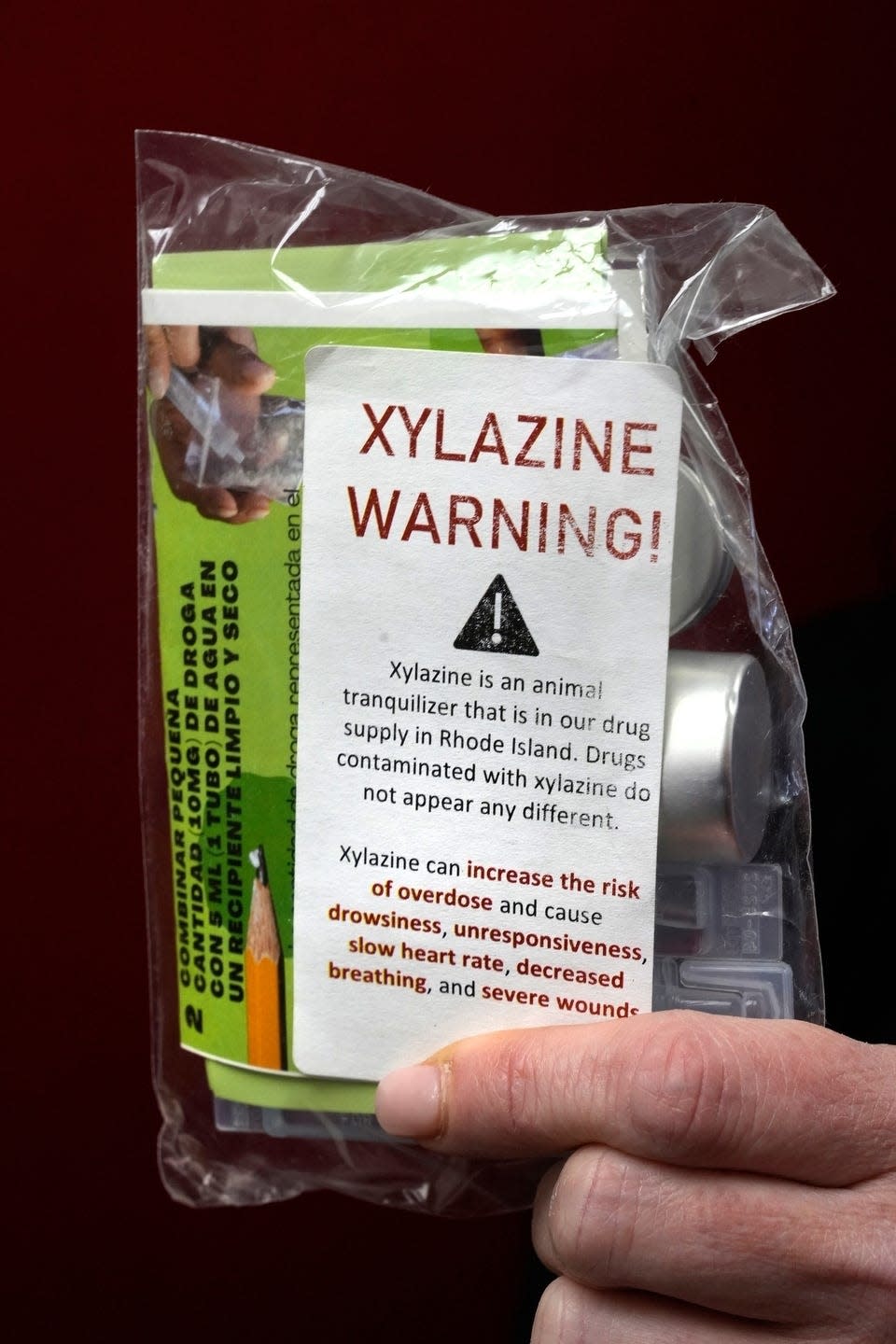
There is a simple way to check for the animal sedative in a personal drug supply: xylazine test strips, which became available in March. But most states consider them illegal drug paraphernalia.
Soria, from the Crossroads Center, said he can't provide xylazine test strips to patients because they’re considered paraphernalia. He said that “has to change.”
In the Cincinnati area, Hamilton County, Butler County and Northern Kentucky health departments are handing out the strips at safer drug-use sites, regardless of their legal status.
“We encourage all our clients to test all their opiates,” said Sharona Bishop, a Butler County General Health District harm reduction specialist and advocate.
Ohio in April changed its drug paraphernalia law to make it legal for people to test their drugs for fentanyl. But Bishop said there needs to be a blanket law that allows testing, “so whenever a testing strip comes out, it is legal to have and use.”
A federal bill introduced in July would stop states from prohibiting the distribution or use of fentanyl and xylazine strips. The bill has not received a vote in Congress.
Nationwide warning: Federal Drug Enforcement Administration warns of xylazine threat

For now? Triage.
In the meantime, those watching the xylazine crisis evolve in the Cincinnati area say they’re trying to keep people safe and alive.
“Most of my patients are still trying to avoid xylazine, but this will pass as they lose their fear, just like the fear passed with fentanyl use,” said Soria.
For her part, McNamee is vigilantly watching for people who come to Butler County’s sites with unusual ulcers or discolored skin.
“I just want to help anyone I can, so the sores don’t worsen,” McNamee said. “I would hate to see anyone lose a limb.”
Dispatch reporter Bethany Bruner contributed to this story.
This article originally appeared on Cincinnati Enquirer: Animal 'tranq' embedded in Ohio and Kentucky fentanyl supply

