NY failed to protect disabled group home residents from COVID, comptroller finds
- Oops!Something went wrong.Please try again later.
- Oops!Something went wrong.Please try again later.
A lack of preparation for a pandemic, confusing and missing guidance from the Office for People With Developmental Disabilities and growing staff shortages made COVID all the more hazardous for people with developmental disabilities who live in group homes and similar facilities, an audit by the New York state comptroller found.
The numbers show the cost: 657 COVID-related deaths occurred among people with developmental disabilities in New York's residential facilities prior to April 5, 2022, the period that audit focused on. (The latest OPWDD data show that there have been 707 COVID-related deaths of residents in group homes and other care facilities as of March 2023; 51 staff members also have died of COVID-related causes.)
About 34,117 New Yorkers live in residential settings overseen by OPWDD; about 83% live in facilities operated by nonprofit agencies, with the rest operated directly by OPWDD.
Supports for people with developmental disabilities also suffered. Between March 2020 and November 2021, 81 group homes were closed or temporarily closed due to staffing shortages, the audit reports. Day programs were halted.
Families of people with disabilities say much of that programming has not returned.
“Group homes are supposed to offer people with developmental disabilities safe places to live as independently as possible,” state Comptroller Tom DiNapoli said. “Inconsistent emergency management coordination and oversight put residents, families and staff in harm’s way.”
The comptroller urged OPWDD to act “before the next public health emergency.”
OPWDD spokesperson Erin Silk said COVID was unprecedented.
“During a global pandemic, OPWDD implemented best practices across facilities to minimize infections and satisfy state quarantine and isolation guidance, while keeping those residents in group homes safe and connected with loved ones," Silk said. "While the ever-changing nature of the public health emergency demanded agility in implementing New York State Department of Health and CDC guidance, OPWDD is proud of the efforts that were made to sustain continuity of services while ensuring health and safety during this unprecedented, worldwide event.”
The current OPWDD commissioner, Kerri Neifeld, became acting commissioner in November 2021, after the departure of Dr. Theodore Kastner, and was confirmed as permanent OPWDD commissioner in March 2022.
State budget: Can workers who aid people with developmental disabilities finally get a wage increase?
Comptroller: Early intervention delays hurt kids
Brick It Again! Lego resale store provides job training for people with disabilities, fun for all
Where did OPWDD fall short during COVID?
Most group homes didn't get key information: OPWDD issued important guidance for COVID safety, but only sent the information to eight intermediate care facilities that OPWDD operates. That left 6,921 facilities that serve about 99% of residents out of the loop.
The comptroller's report did not establish a causal relationship between OPWDD’s actions and COVID cases. But, it notes, there were 12,895 COVID cases and 649 deaths in facilities that didn't get the guidance, and 33 COVID cases and four deaths for the eight intermediate care facilities.
Emergency plans unchecked: OPWDD requires all facilities to have emergency plans in place. While the state agency’s own plans addressed risks from pandemics, even before COVID hit, OPWDD didn’t ensure that nonprofit group homes had made similar preparation plans.
The comptroller found that while safety plans are reviewed every three years, OPWDD didn’t look at things like infection control practices or public health response plans.
PPE shortages: OPWDD had a stockpile of PPE, but it ran out fast. Nonprofits were often left to find their own.
With the inability for many direct support workers to socially distance from people who need help with feeding, dressing and toileting, a lack of PPE left everyone in the facility vulnerable to COVID spread.
COVID surveys ineffective: OPWDD surveyed group homes in May of 2020 to gauge the pandemic response. But investigators only visited 22% of homes. “Further, surveys often lacked meaningful observations, and staff at certified group homes were not required to take refresher trainings on infection controls,” the audit states.
Visitation rules, other issues plagued facilities during COVID
OPWDD’s response to COVID has drawn criticism prior to the comptroller's report.
In April 2020, OPWDD issued an advisory mandating certified residential facilities make a plan to accept group home residents who had been treated in a hospital for COVID-19 and deemed medically able for discharge, as long as they were asymptomatic.
The guidance was similar to then-Gov. Andrew Cuomo’s March 2020 Department of Health advisory to nursing homes to accept asymptomatic residents who had been hospitalized for COVID. Critics have said that mandate lit the fuse for the explosion of nursing home fatalities.
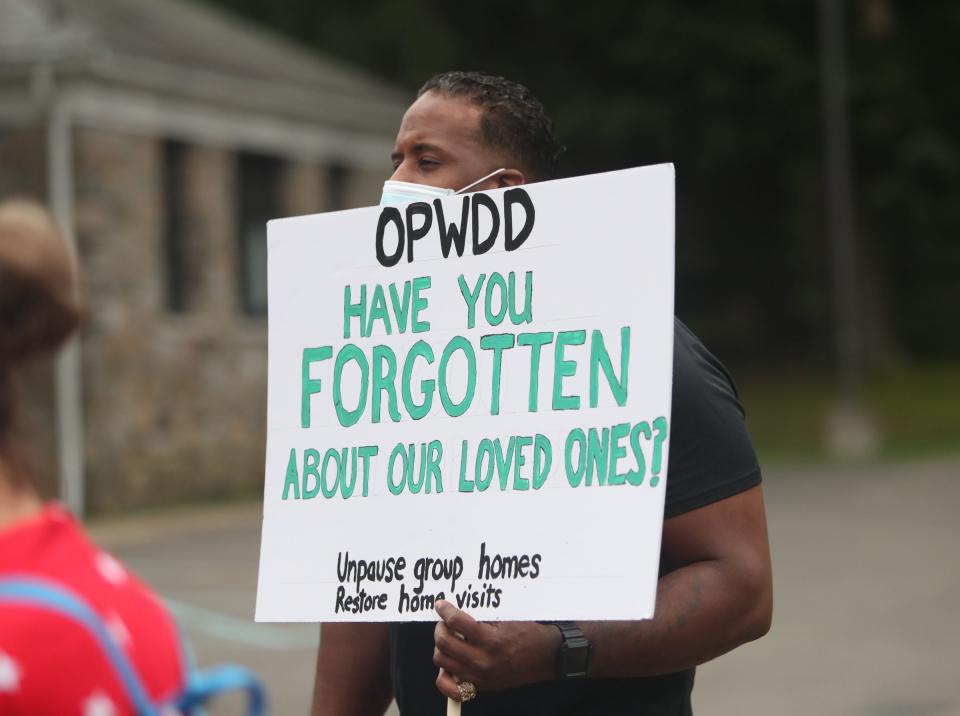
Then, as Cuomo's Reopen NY plan was laid in spring 2020, group homes were left out. Residents remained unable to go home or out into the community and families unable to visit until July 2020.
Families said the exclusion made little sense. Workers were coming in and out, and even going between group home facilities to help cover staff shortages, adding to the risk of COVID spread.
Russell Snaith, a founder of New York Alliance for Developmental Disabilities, said the group formed in response to the extended lockdowns. "It put emotional distress on the individual served," Snaith said, many of whom could not understand COVID restrictions overall.
The Snaiths, who live on Long Island, decided to move their 27-year-old son, Dylan, home from his group home during the four-month shutdown, because they knew "it would break him." But many families couldn't do that.
Low wages for workers hurt system, residents
Snaith said the comptroller's audit contains valuable information. But OPWDD must also take the next step and get lost programs back on track.
"All of the restrictions have been eased so the only barriers from resurrecting these programs is staff," Snaith said.

NYADD, with more than 10,000 members, is now tackling wage disparities for direct service professionals, known as DSPs, who help people with developmental disabilities live as independently as they can. Years of neglect by the state has left workers earning just above minimum wage.
Gov. Kathy Hochul's Fiscal Year 2024 budget plan, now in overtime negotiations, would provide a 2.5% cost-of-living reimbursement increase, called a COLA, for DSP salaries; the Senate and Assembly want 8.5%. Family advocacy groups like NYADD want more.
The state sets DSP wages through Medicaid reimbursements to the agencies that employ them.
Snaith said the state has allowed DSP wages to drop for more than a decade, compared to other occupations. Agencies now deal with 30% vacancy rates and 30% staff turnover rates.
"It came home to roost," Snaith said.
Tara Klein of Pleasantville, a NYADD member, said the comptroller's report should be a wake-up call to gird the system before the next crisis. One way to do that, she said, is by making sure staffing is strong.
"Governor Hochul now has the opportunity to right these wrongs by funding OPWDD providers with the COLA," Klein said, "and paying this dedicated DSP workforce a living wage to support New York's most vulnerable residents with disabilities."
Nancy Cutler writes about People & Policy. Follow her on Twitter at @nancyrockland.
This article originally appeared on Rockland/Westchester Journal News: NY failed to protect disabled group home residents from COVID

