A NYC hospital has figured out how to turn sleep apnea machines it got from Elon Musk into ventilators for coronavirus patients

Mount Sinai
New York is running short on ventilators, the breathing machines that could be the difference between life and death for some coronavirus patients.
Mount Sinai Hospital in Manhattan has figured out a way to turn sleep apnea machines into ventilators after receiving a donation from Tesla CEO Elon Musk in late March
Dr. Hooman Poor, who helped convert the machines, told Business Insider that after a few tweaks, "there was really no reason why this couldn't work."
Instructions and protocols developed by the hospital to modify and use these machines have now been shared with other hospitals around the state and country
New York is running out of ventilators. To address the shortage, doctors are getting creative.
At Mount Sinai Hospital in Manhattan, a team of healthcare workers developed a way to turn sleep apnea machines, devices typically used to help people who have trouble breathing while they're asleep, into ventilators.
The hospital received a donation of 200 sleep apnea machines from Tesla CEO Elon Musk in late March. Since then, staff has worked to turn the devices into tools that could help patients with trouble breathing, a common symptom of COVID-19, the disease caused by the coronavirus.
The hospital plans to use them for patients whose breathing problems aren't as severe as some other COVID-19 patients.
Currently, Mount Sinai has 300 of the machines on hand and has modified 30 of them. Conversion of the remaining 270 will be finished in the next few days, and the hospital expects an additional 1,000 to arrive in the near future.
The idea is to use them to stave off a worst-case scenario: running short on ventilators as the number of coronavirus cases in New York City reaches a peak.
"The one horrific decision I never want to have to make is who gets a ventilator and who doesn't," Dr. Hooman Poor, a physician at Mount Sinai who worked on the project, told Business Insider. "That's a horrifying situation. It's an ethical dilemma that has been discussed widely in this pandemic and having these machines available would reduce the likelihood that we would ever have to make that decision."
'There was really no reason why this couldn't work'
When the hospital received the donation, healthcare workers discussed whether these machines — which also help people breathe, albeit in usually less critical conditions — could be used to help coronavirus patients.
"There was really no reason why this couldn't work," said Poor, who's an assistant professor of pulmonary, critical care and sleep medicine at the Icahn School of Medicine at Mount Sinai.
There were some tweaks that the hospital had to make.
One of the biggest concerns with using sleep apnea machines as ventilators for coronavirus patients is the risk of the machine aerosolizing the virus, spreading it more readily and putting healthcare workers at increased risk of catching it.
"We had to deal with the fact that we're dealing with a highly contagious virus," Poor said.
The conversion process
With standard ventilators, air that is breathed out by the patient is sent to an exhalation port that prevents the air — that is potentially contaminated with a virus — from directly entering the room.
Mount Sinai
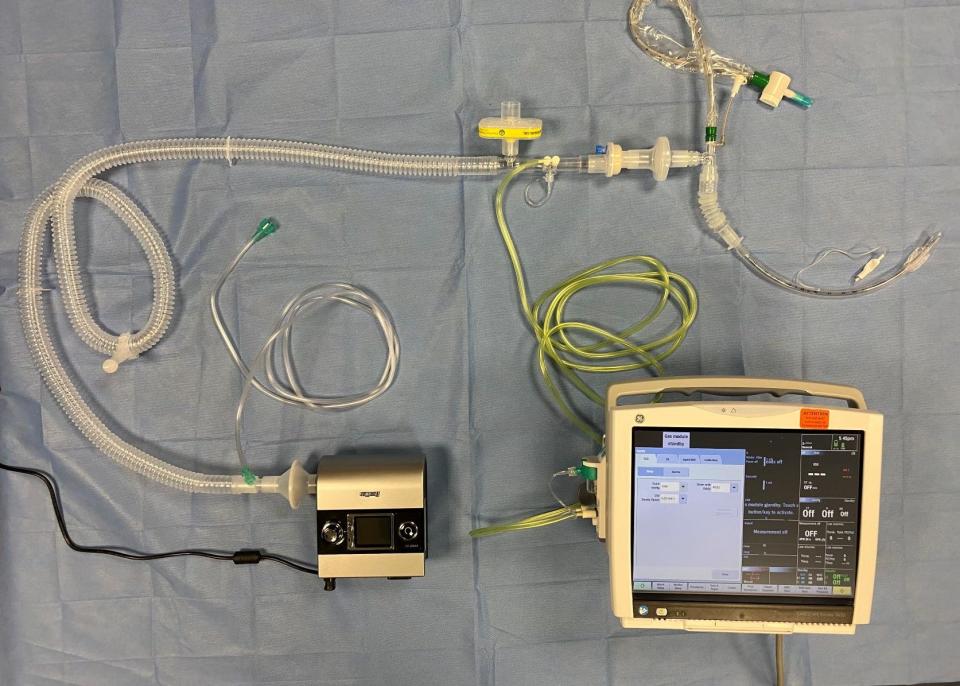
Poor said he and a team of around 15 healthcare workers modified the sleep apnea machines to perform a similar function by putting a viral filter on the exhalation port of the machine, which would make sure the air breathed out by the patient would go through the filter instead of directly into the air in the room.
The conversion from sleep apnea machine to ventilator is simple, Poor said. With the instructions they've currently laid out, it would take around 10 minutes to modify each machine, though they are only able to convert bilevel machines, also known as BiPAP machines.
CPAP machines, also used by people with sleep apnea, can't be converted in the same way.
Other hospitals have gotten creative as well. Stanford has repurposed snorkeling masks as reusable PPE for healthcare workers and The University of Nebraska Medical Center has said it is using UV light to disinfect and sterilize N95 masks so they can be resued. Other medical centers and hospitals around the country, that are facing or expecting serious shortages, are using household materials to design makeshift masks as short-term PPE replacements.
At Mount Sinai, the reconfigured machines can alert healthcare workers if there is a problem with the patient's air flow and can be accessed and controlled from outside the patient's room, allowing clinicians to make minor changes to the ventilator's settings without having to go into the patient's room. This helps to preserve personal protective equipment for healthcare workers.
New York's need for ventilators
New York, which has become the epicenter of the coronavirus pandemic in the US with over 130,000 confirmed cases as of Tuesday morning, is running short on ventilators. Governor Andrew Cuomo has publicly asked for help from the federal government and other states.
Ventilators could be "the difference between life and death," Cuomo said at a press conference late March, where he stressed the state's need for the machines.
Last week, the state received 1,000 from billionaires Jack Ma and Joseph Tsai, the founders of Alibaba, a Chinese e-commerce company. States like California, Washington, and Oregon have pledged to send more.

Mount Sinai
A safer option
The reconfigured ventilators are safer than splitting ventilators to serve multiple patients at the same time, according to Poor. That's been suggested as a last resort option that some hospitals have been preparing for as ventilator supplies run low.
If a hospital were to connect two patients to a single ventilator, they would, first of all, have to match patients closely in terms of condition and the amount of oxygen and pressure they'd require. If one of these patients were to get suddenly worse, however, they would suddenly need different settings on the ventilator than their partner-patient, causing problems.
Though the sleep apnea machines-turned-ventilators are useful for patients who may be on their way to recovery, they are not powerful enough to stabilize patients with severe respiratory issues. Regular ventilators, which are more powerful, will still be needed to treat patients with more severe breathing problems.
Read the original article on Business Insider

