Ohio ranks 9th in US for potentially deadly, drug-resistant fungal infection
The Centers for Disease Control and Prevention issued a warning this week about a drug-resistant fungal infection it calls an “urgent threat," but central Ohio health officials say basic precautions can help prevent it from spreading.
Ohio ranks ninth of 29 states in the U.S. where infections caused by Candida auris, or C. auris, yeast was identified in 2022, with 79 infections, according to the CDC.
First reported in the United States in 2016, the number of infections has grown nationwide to 3,270 through 2021, with the most rapid hike happening in 2020-21, according to a study published Monday in the Annals of Internal Medicine, when the number of times the fungus was detected — but did not cause infection — tripled to a total of 4,041.
The CDC cited many reasons for the increase, including poor general infection prevention and control practices in health care facilities, enhanced efforts to detect cases and strained health care and public health systems during the COVID-19 pandemic.
Candida auris fungal infections:'Urgent threat': CDC warns against Candida auris, a drug-resistant fungus invading health care facilities
The fungus spreads through contact with surfaces and equipment, especially in health care facilities, such as hospitals and nursing homes, or people who are infected, according to the CDC. Those at highest risk are people who have recently spent time in a nursing home and have feeding or breathing tubes or central venous catheters.
Other risk factors include recent surgery, diabetes and broad-spectrum antibiotic and antifungal use.
What is Candida auris, or C. auris?
Candida auris is a drug-resistant fungus that can cause outbreaks in health care facilities, according to the CDC.
The fungus can infect the bloodstream and even cause death by invading the blood, heart and brain, the agency said. More than 1 in 3 patients die from such an infection.
Experts say the pathogen is also dangerous because it’s often resistant to antifungal medicines commonly used to treat infections. It’s also difficult to identify without specialized laboratory technology, and is often mistaken for other infections.
The agency said C. auris was first identified in 2009 in Asia and has quickly spread throughout the world. Since it began spreading in the U.S. in 2015, reported cases have increased more than 300%.
Candida auris infection symptoms
C. auris doesn’t always cause infection and can be carried on a patient's skin, the CDC said, allowing easier spread to others.
But when it does cause infection, the agency said, it may be difficult to identify because it most often occurs in patients who are already sick with other diseases and exhibiting symptoms.
The CDC says fever and chills that don’t improve after giving antibiotics are the most common symptoms of C. auris.
How common is Candida auris in Ohio?
The Ohio Department of Health declined The Dispatch's request for an interview, but provided a brief overview of the fungus' prevalence across the state, which first reported a case in 2020.
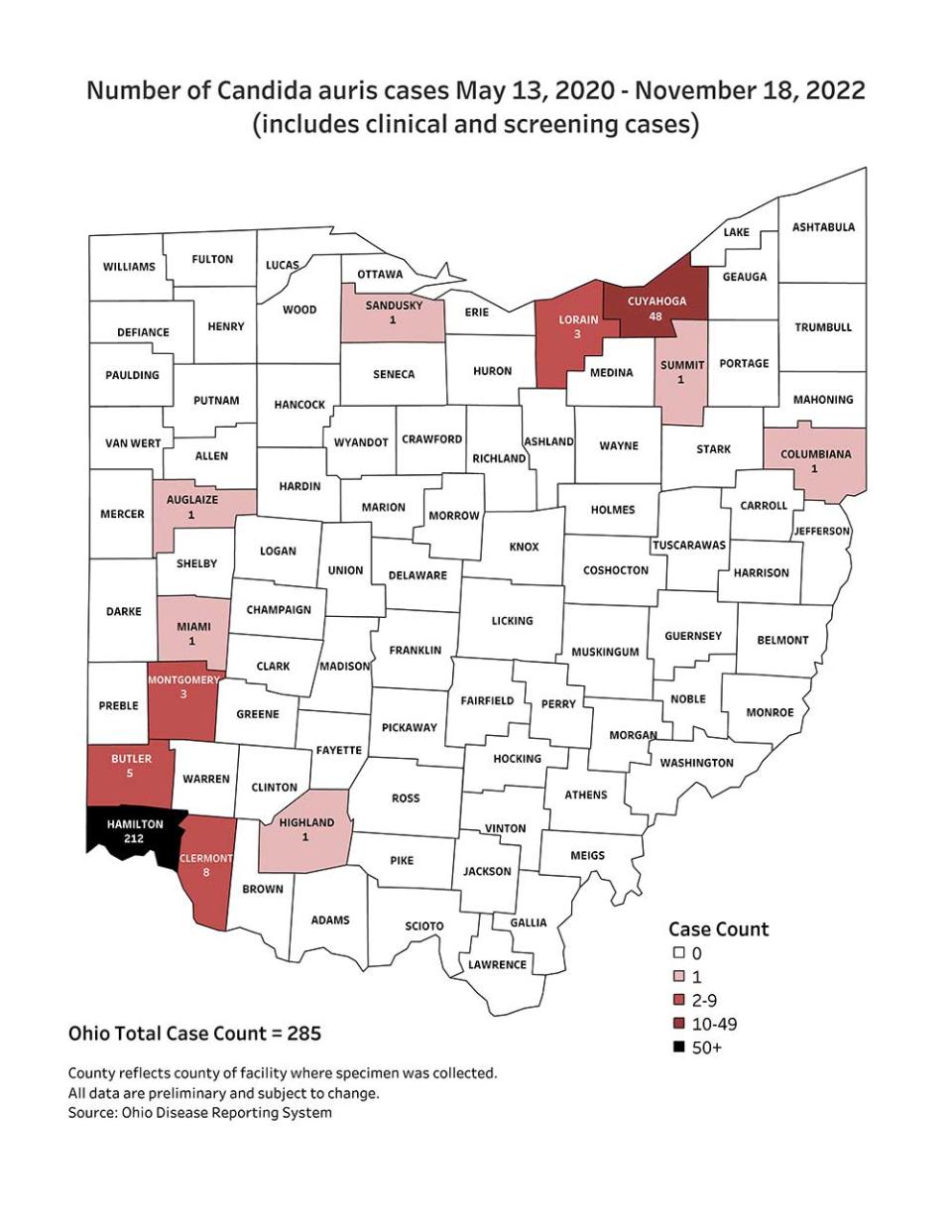
From May 13, 2020, to Nov. 18, 2022, there were a combined 285 cases of C. auris in Ohio, according to state Health Department data. Of those, 95 cases resulted in infections, all but two of which were near Cincinnati, Cleveland and Dayton.
In February, Columbus Public Health identified one case within its jurisdiction in which the person was not sick and only found out they had the fungus after getting a random skin test, spokesperson Kelli Newman said.
"Like all things, just keep your hands and surfaces clean because we can carry it on our skin," Newman said. "We all have yeast on our skin. For the average person, it's not going to make you sick."
Fighting fungal infections
Experts say fungal infections, including C. auris, also are difficult to treat because antifungals can be harmful to humans.
That makes prevention key, said Lance B. Price, professor of environmental and occupational health and the founder and co-director of the Antibiotic Resistance Action Center at George Washington University.
“The scary thing about Candida auris and any of the drug-resistant fungal infections is just how difficult it is to find good, safe antifungals because people and fungi are built of the same stuff,” said Price, who is not affiliated with the CDC study.
Antifungal agents also are being overused in the agricultural setting, he said, which may contribute to more drug-resistant strains.
Study authors say the rise in C. auris cases may be a result of increased surveillance efforts picking up more cases, decreased prevention efforts because of a burdened health care system during the COVID-19 pandemic, or both.
“Hospitals have to step up and screen patients for drug-resistant strains, isolate them, be on top of their game when it comes to infection control," Price said.
nshuda@dispatch.com; @NathanielShuda
@AdriannaUSAT
This article originally appeared on The Columbus Dispatch: Ohio ranks 9th in US for drug-resistant fungus Candida auris infections

