One chart can tell you whether you actually need a booster shot
Booster shots are now available to a broad swath of people in the US who are fully vaccinated.
But the truth is that most Pfizer and Moderna recipients probably don't need a third shot yet.
Data suggests people over 65 and J&J recipients would benefit from a boost immediately.
Booster shots have arrived in the US.
Many adults who have been fully vaccinated with Pfizer, Moderna, or Johnson & Johnson's COVID-19 vaccines can now boost their initial regimens with an additional jab of whichever vaccine brand they want, though that extra shot is voluntary, for now.
But not everyone needs a booster shot yet, and the truth is that most Americans probably don't.
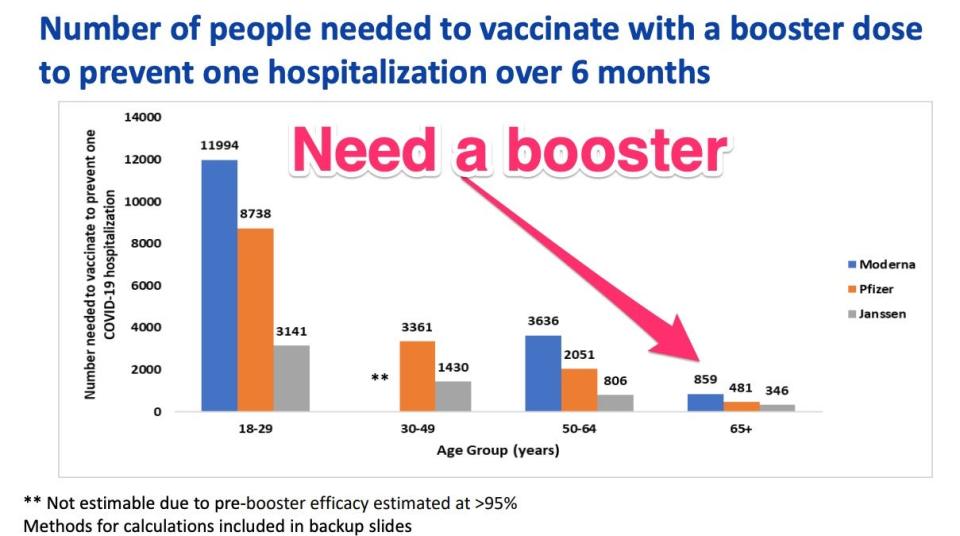
A chart below displays this idea well, showing how many booster shots it would take to prevent a single COVID-19 hospitalization over six months.
It was part of a wide array of data reviewed by an independent advisory committee to the Centers for Disease Control and Prevention last week, showing that boosters should be most heartily recommended for older adults, as well as everyone who's had the J&J vaccine. For everyone else - even those with comorbidities - the evidence is far flimsier.
"This isn't about who deserves a booster; it's about who needs a booster," Dr. Matthew Daley, a CDC advisory committee member from Kaiser Permanente Colorado, told the agency at its meeting on Pfizer boosters, stressing that people over 65 and long-term care facility residents should be prioritized.
Who's eligible for a voluntary booster shot?
The new CDC recommendations are pretty broad, which means a majority of fully vaccinated adults are technically eligible to get jabbed again.
Extra shots are available to:
All J&J vaccine recipients
Pfizer and Moderna vaccine recipients 65 years and older
Pfizer and Moderna vaccine recipients 18 and up who live in long-term care settings
Pfizer and Moderna vaccine recipients 18 and up who have underlying medical conditions
Pfizer and Moderna vaccine recipients 18 and up who live or work in high-risk settings
Pretty much every J&J recipient could use a boost
The 15.4 million adults across the country who have received Johnson & Johnson's vaccine could likely all benefit from a booster shot (at least two months after their initial vaccine), regardless of their age or immune status.
Though they are a small fraction of the fully vaccinated in the US (8%), real-world data is showing they are at risk.
J&J's single-shot vaccine is clearly not protecting them from hospitalization and death as well as the two-shot mRNA vaccines.
People under 65 with Pfizer or Moderna don't really need boosters, data suggests
A plethora of real-world data on Pfizer and Moderna's COVID-19 vaccines is showing that they're both doing quite well at protecting people from serious illness.
In fact, Moderna's vaccine was so effective at preventing hospitalizations among adults aged 30-49 (more than 95%) that federal scientists couldn't even calculate what effect a booster shot might have on their risk of hospitalization, because it is already so slim.
There are always individual differences to consider, but generally speaking, boosters aren't giving young people much extra benefit right now.
For adults 65 and up, the benefits of a boost are clearer. Fewer than 860 adults in the 65+ age group would need to be boosted with Moderna to prevent one hospitalization, and fewer than 500 adults who got Pfizer would need to be boosted to prevent the same.
Why older and immunocompromised people could use a boost
Boosters will certainly help better protect older adults from infection (their immune systems are naturally weaker and in need of more frequent and stronger boosts).
Third (and even fourth) shots may also help some immunocompromised patients who don't respond to a first or second dose (though some immunocompromised people will likely never achieve great vaccine protection, so they need others to get vaccinated to protect them).
CDC advisors said the real reason boosters are even being considered for younger front-line workers, like hospital staff, is because there is such a long line of critically ill unvaccinated patients to care for. Hospitals can't afford to have any vaccinated staff out sick while COVID-19 is spreading so fast among the unvaccinated.
While there is early evidence that boosters might cut down on transmission or mild illness, no booster shot of any vaccine will ever completely eliminate the risk of a breakthrough infection while community transmission is high, and it's unreasonable to expect it to do so.
Boosters might be needed for everyone someday as vaccine protection wanes, but that day hasn't come yet.
Vaccines are saving lives, even without boosters
Despite the fact that vaccines work to prevent serious outcomes in younger adults, COVID-19 was the leading cause of death for people ages 35-54 in September, according to a recent Kaiser Family Foundation analysis. Almost all of those deaths could have been prevented if unvaccinated people got vaccinated.
"We're fighting a pandemic, and it's not because people got two doses of vaccine," Dr. Helen Keipp Talbot, a CDC advisory committee member from Vanderbilt University, said at a recent meeting on boosters.
Federal data suggests that basically all of the life-threatening cases of COVID-19 in fully vaccinated people are in elderly patients over the age of 80 (though there are a few in the 65-79 age group too.)
The bottom line
If you're over 65, immunocompromised, or got J&J's vaccine, you probably could benefit from a booster.
For everyone else, passing around boosters like Halloween candy might be like putting "lipstick on a frog," Talbot said.
Read the original article on Business Insider

