Organ transplant milestone: As US crosses 1 million mark, advances offer hope for millions more
Richard Herrick, 23, was facing certain death in 1954 when his identical twin, Ronald, agreed to give him a kidney.
Organ transplants had been contemplated since at least the time of the ancient Egyptians, but the idea was a fantasy. Richard's immune system, however, had no trouble accepting his brother's kidney, and he lived for eight years as the world's first successful organ transplant recipient.
Friday, the United States passed another milestone: 1 million successful solid-organ transplants since Herrick's. Most have been kidneys, followed by livers, hearts and lungs.
"To have the ability and the science and the technology to transplant an organ from one person to another so that person has another chance to live is nothing short of a miracle," said Barry Massa, president of the Association of Organ Procurement Organizations. "Without the generosity of people who said yes to being a donor … none of this would have been accomplished."
Half of those transplants came during the 53 years after Herrick's and half in just the past 15, according to data from the nonprofit United Network for Organ Sharing, which provided the count.
Last year, for the first time, more than 40,000 solid organs – more than 100 a day – were transplanted.
At that pace, the next 1 million transplants will take only 25 years – and probably far less because of medical innovations under development, said David Klassen, the network's chief medical officer.
"Right now is a really exciting time, because there is so much going on in so many different directions," Klassen said. "We're at an inflection point, a hinge of history. I think things are going to evolve fairly quickly and change directions quite significantly."

The speed-up has been possible as more surgical teams around the country have developed the expertise and organ procurement organizations and transplant hospitals have shared best practices. Advances in technology have allowed organs to be kept longer outside the body. And – tragically – the nation's opioid epidemic has killed more otherwise-healthy young people, providing more donors.
Still, more than 60,000 Americans on an organ transplant list were unable to get one last year because of limited supply. And many more never made the list, because they were considered too big a risk for the limited supply, either because of advanced age or prior behavior.
For them, hope lies in resolving the two lingering problems with organ transplantation: supply and immunosuppressive medication.
Immunosuppressive medication
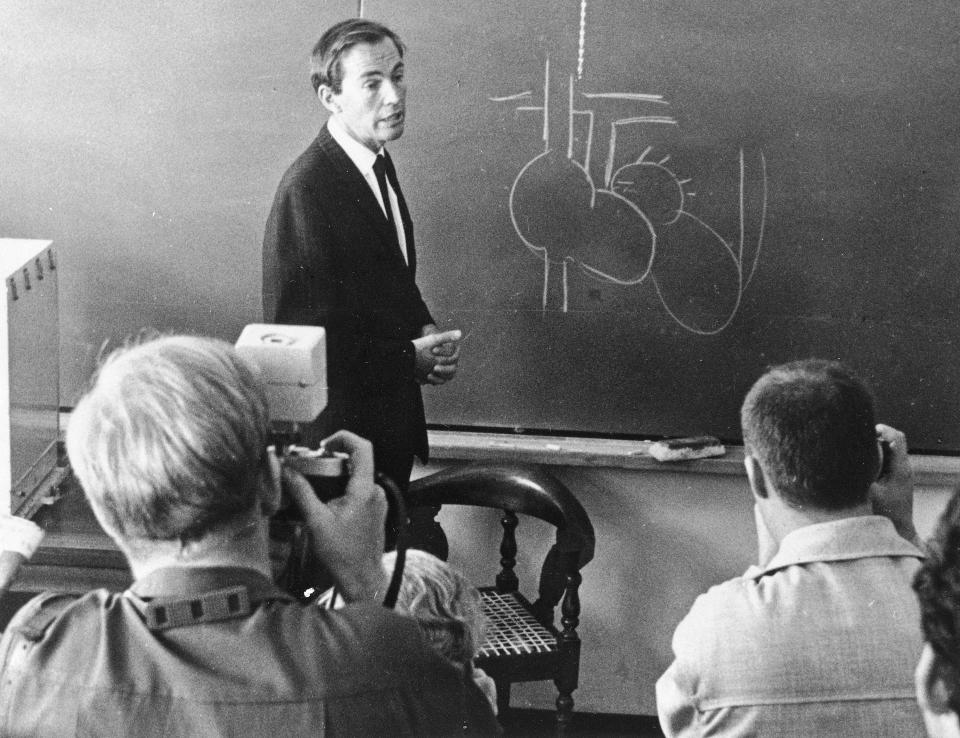
As of 1963, fewer than 10% of transplant patients survived longer than three months after surgery. That was the year transplant surgeon Tom Starzl showed he could replace radiation therapy with a combination of drugs to tame immune system rejections.
Within a year, the number of transplant programs in the United States jumped from just three – in Boston, Richmond, Virginia, and Starzl's in Denver – to more than 50.
Another transformation took place after the discovery in 1976 of cyclosporine, an immune system suppressing drug derived from fungus, followed by the approval in 1989 of tacrolimus, which suppresses the immune system even more effectively.
But the medications that keep people from rejecting organs also doom transplants as damage accumulates over time.
"They're both lifesaving and life-ending," said Dr. Jacob Schroder, a heart transplant surgeon at Duke University School of Medicine in North Carolina. "It's such a delicate balance between rejection and infection."
On average, a kidney or heart from a deceased donor lasts about 12 years – enough for an older person to reach a typical life span, but a sword of Damocles hanging over the heads of younger ones, who will at some point need another transplant. Each transplant gets harder on the body as it struggles to cope with yet another foreign organ.
Most transplant centers won't give a heart to anyone over 70 because of the risks, Schroder said. "If you're 50, your body will tolerate both the transplant and the recovery and the immunosuppressive drugs better than if you're 70."
Paying for the medication also has been a challenge.
Medicare and most insurance companies have covered immunosuppression only for three years after a transplant. At an average cost of $10,000 to $14,000 a year, it's a huge burden for people who must keep taking the medication indefinitely. New laws will require government coverage as of January.
Increasing supply
People have two kidneys and need only one, so they can give one away. About 15% of kidney recipients receive a kidney from a live donor, usually a sibling with a closely matched immune system, or a stranger.
That isn't an option with hearts.
At least 300,000 Americans a year could benefit from a new heart, Schroder said.
But only 3,800 Americans received a new heart last year – a record high, and an increase from about 2,500 a decade or so ago.
"It is an ever-evolving process to try to get the hearts to the people who need them the most," Schroder said.
The nation's opioid epidemic has made more hearts available, he said.
Typically, organ donors are people who meet the strict definition of brain death, Schroder said, with no blood flow to the brain, among other criteria. But some people have neurologic injuries "that will not allow them any meaningful recovery but do not meet the very strict criteria for brain death," he said.
Since Dec. 1, 2019, hearts from those patients have become available for transplant with their family's consent.
Donors after circulatory death are generally younger and died from something other than heart failure, often opioid overdose, so their hearts are particularly healthy. Last year, 205 such hearts were used for transplant, and so far this year there have been 188 transplants from donors after cardiac death, up from seven in 2019, according UNOS the organ sharing network.
Studies show that five-year results using these hearts "are at least equivalent to normal brain-dead donors," said Schroder, who led a recent one. "We should be able to increase the donor pool at least by 30% (using these hearts). Most likely higher than that."
Supply has also expanded thanks to a cure for hepatitis C, a potentially lethal disease common among intravenous drug users. Now, with treatment, people can receive a hepatitis C-infected heart and be treated and recover before they have any symptoms. HIV-positive patients can now also receive hearts from donors who had the infection.
"People are being more and more aggressive about accepting hearts that 10 years ago people would not have accepted, knowing that those hearts actually are fine," Schroder said. "The risk is actually relatively low to die from a heart-related complication."
Still, of all the hearts offered for transplant, only about one-third are used out of concern for their viability. Schroder helped prove the effectiveness of an approach that improves the quality of donated hearts and allows them to last longer.
"That technology is very exciting," Klassen said.
Surgeons get concerned about the heart if it is preserved on ice for more than four hours, Schroder said.
By using a portable heart-lung machine, so-called ex vivo perfusion can extend that time, mimicking what happens inside the body by keeping blood flow to the heart. Using this device, instead of just putting the heart on ice, has allowed Schroder's team to bring organs from Puerto Rico and Wyoming to North Carolina despite the distance.
"We've shown excellent results," he said.
Improving equity in transplants
Historically, white patients have been more likely to get a new organ than patients of color with the same health status. But that's starting to change.
Although Black people are more likely to suffer severe kidney disease, a race-based calculation may have prevented African Americans on the wait-list from being properly prioritized for organs. That system's removal "should allow more African Americans and minorities on the wait list to receive their kidneys," said Massa, also executive director of the LifeCenter Organ Donor Network in Cincinnati. "It was a big step."
Still, he said, people without financial means have a tough time making it onto organ wait lists. They lack insurance, can't get to regular medical appointments or can't leave work to go to them. "They have a lot of things going against them even to be listed in the first place," Massa said.
Geography also can create inequities, he said. Because organs can travel only so far, "I'm sure there are some disparities," with people in remote rural areas having less access to organs than those in major cities. Overall, though, the organ donation rate is relatively consistent across the country, he said.
Donations also are climbing among people of color. In the past five years, rates of deceased donors have jumped more than 30% among people who are Black, Hispanic and Asian. "We have a long way to go, but I think we're seeing really good, positive momentum," Massa said.
To get even more people to donate, Massa said, his organization and others need to "dispel myths and misconceptions as well as rebuild that trust within the health care system."
The Association of Organ Procurement Organizations is working with Historically Black Colleges and Universities to encourage more students of color to enter careers in transplantation and to register as organ donors.
Increasing transplants and transplant equity, Massa said, still depends on having "more people say yes."
"It's incumbent upon us to get that word out, to educate that community to see the benefits of registering as an organ, eye and tissue donor."
(To become an organ donor, register at registerme.org.)
Saving lives, expanding protection
Jessica Davenport's son, Kruz, now 9, was slowing dying from a rare genetic disorder that was destroying his kidneys and weakening his immune system.
Tests revealed that his little sister, Paizlee, who appeared healthy, had the same genetic disorder – a 1 in 80 million stroke of bad luck, as Davenport puts it.

"We wanted answers, but we didn't want that answer," she said.
She was discussing her children's condition with doctors at the Stanford School of Medicine when one suggested they first get a kidney transplant and then a stem cell transplant to repair their immune system.
"No, no, no. We need to do the stem cell transplantation first," blurted out Dr. Alice Bertaina, surprising even herself. Her research suggested that if the children got a stem cell transplant first, they might be better able to survive the kidney transplant. Best of all, they might not need immunosuppressive medications.
So in 2019, Kruz got a bone marrow transplant from his mother and then one of her kidneys. Two years ago, his sister got the same from their father. A third, unrelated child also received a double donation. None of the children need immunosuppressive medication, and there's no obvious expiration date on their new organs. (A paper on their medical procedures was published this summer.)
Both Davenport children also have dwarfism – neither is ever likely to reach 4 feet – and Kruz has hip problems and some neurological problems. They're still at risk for stroke, but not for kidney failure or severe infection.
"They've been through so much, and they have joy in their hearts and they love everybody," Davenport said. "I always knew they were going to change the medical world."
It isn't practical to give a stem cell transplant to everyone who needs a new kidney, Bertaina said, but enabling three children to be immunosuppression- and rejection-free offers "hope for many patients that we didn't have hope for, and that's the most important part."
David Sachs, a transplant researcher at Columbia University in New York and Massachusetts General Hospital in Boston, said the procedures confirm the potential of using donor cells to eventually move away from organ-damaging medications.
"I'm delighted to know this worked so well," he said.

Looking toward the future
Sachs, 80, has been working most of his life to increase organ supply and reduce the need for immunosuppressive medication.
He showed years ago in a small trial that he could induce tolerance to a foreign organ by providing bone marrow from the donor along with an experimental drug.
The first patient was 12 years old when she received an organ from her father. Despite a 22-pill-a-day regimen, the organ was failing by the time she graduated from college. Following Sachs' protocol, she received an organ from her mother, along with the experimental drug and bone marrow. She has survived 17 years, most of the time without immunosuppressive medication.
But the drug was taken off the market nearly a decade ago, which halted trials. A new company recently purchased it, and Sachs is hopeful research will begin again soon.
Sachs, who splits his research time between Columbia University and Massachusetts General Hospital, has long been working toward the possibility of xenotransplantation, using animal organs in people. In 2005, he oversaw the first gene edits to a pig to make its organs less likely to be rejected by a human.
"I started working on this many years ago when a lot of people thought I was crazy," Sachs said.
For several decades, he has thought the field was on the verge of clinical trials – which still haven't started. But last winter, a Maryland man lived for two months with a heart from a gene-edited pig, proving such a transplant was theoretically possible.
In the transplantation field, using animal organs is viewed as a bridge – meant to ease organ shortages while waiting for even more experimental procedures to be developed.
A small number of researchers are exploring the possibility of printing organs with a 3D printer, one layer at a time.
Meanwhile at Stanford, another team is working to get animals to grow human organs rather than using pig organs, which could reduce the need for immunosuppression.
"This could be the future," said Michael Snyder, the Stanford geneticist leading the research.
In a recent paper, the team showed it could take chimpanzee blood cells and turn them back into cells resembling those in an early embryo. They were able to implant the chimp cells into a macaque embryo and get them to grow together.
Eventually, Snyder said, he hopes to remove the genes for a macaque organ and try to grow a chimp organ in its place.
He understands there are ethical questions that arise from such research, but he hopes they can be worked through to allow the science to advance.
As to how soon such a technology might be available, "I'd like to think we're within 20 years," Snyder said. It won't be five years, but he's hopeful it won't be 50, either.
"Things can move faster than you think."
Contact Weintraub at kweintraub@usatoday.com and follow her on Twitter @kweintraub.
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.
This article originally appeared on USA TODAY: US reaches 1 million organ transplant milestone, as advances continue

