Here’s How the Pandemic Finally Ends
The microscopic bundles of RNA, wrapped in spiky proteins, latch on to human cells, hijack them, use them as factories to replicate, and then leave them for dead. It’s a biological blitzkrieg—an invasion so swift and unexpected that the germs are free to jump from host to host with little interference.
Fast forward to the future. Now, when the prickly enemies invade the lungs, they slip past the human cells, unable to take hold. They’re marked for destruction, soon to be surrounded and eliminated. Though some escape through the airways, they confront the same defenses in their next target—if, that is, they can get anywhere near the human cells. There are so few people left to infect that the germs have nowhere to replicate, nowhere to survive.
This is the end of the coronavirus pandemic. And this is how it could happen in the United States: By November 2021, most Americans have received two doses of a vaccine that, while not gloriously effective, fights the disease in more cases than not. Meanwhile, Americans continue to wear masks and avoid large gatherings, and the Covid-19 numbers drop steadily after a series of surges earlier in the year. Eventually, as more and more Americans develop immunity through exposure and vaccination, and as treatments become more effective, Covid-19 recedes into the swarm of ordinary illnesses Americans get every winter.
“It will take two things to bring this virus under control: hygienic measures and a vaccine. And you can’t have one without the other,” says Paul Offit, director of the Vaccine Education Center and an attending physician in the Division of Infectious Diseases at Children’s Hospital of Philadelphia.
The future laid out above is the likeliest scenario for how the pandemic could end, based on interviews with 11 top-level experts who think about the future of those microscopic SARS-CoV-2 particles every day.
They agree there’s a lot of fog left in the Covid-19 crystal ball, but most accept several likelihoods: At least one effective vaccine—hopefully several—will be approved in the U.S. by early next year. Producing and distributing a vaccine will take months, with the average American not receiving their dose (or doses) until at least mid- or late 2021. And while widespread inoculation will play a large role in bringing life back to normal, getting the shot will not be your cue to take off your mask and run free into a crowded bar. The end of the pandemic will be an evolution, not a revolution, the vaccine just another powerful tool in that process.
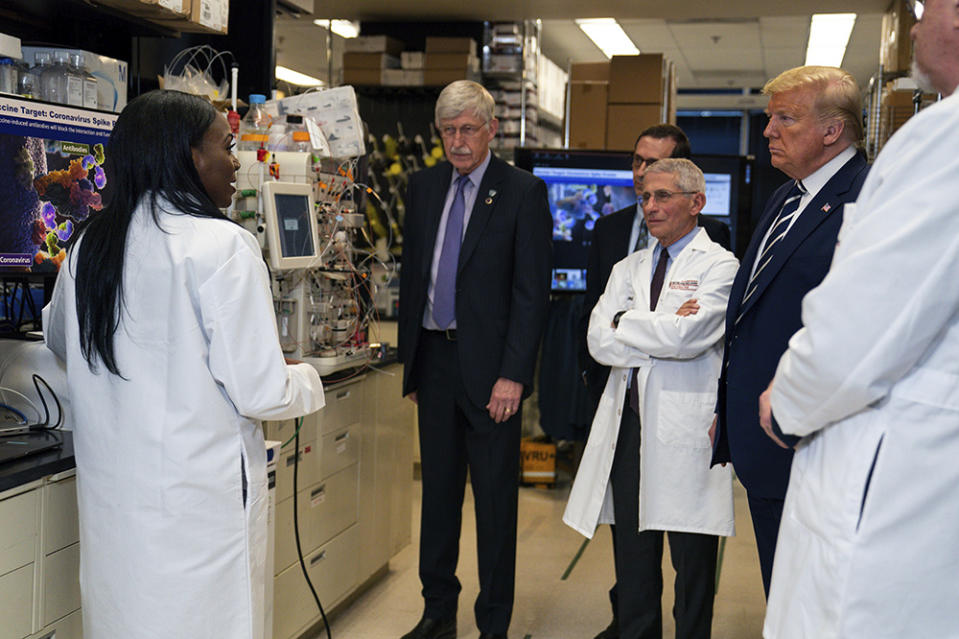
That assessment dramatically contrasts with President Donald Trump’s Panglossian certainty that the U.S. has “rounded the corner” in the pandemic, that a vaccine will be ready by Election Day and that every American can get the shot by April. Most importantly, it contradicts the underlying assumption of Trump’s many proclamations: that life will immediately return to normal after a vaccine is administered.
“I don’t see this pandemic ending as in like, you know, ‘This is the day, the pandemic ended,’” says virologist Angela Rasmussen. “I see this as being a process that will go for a long time, potentially even years.”
Experts’ estimates of the timeline vary, but there seems to be some agreement that the virus could be in decline and under control by the second half of 2021, and that society could see pre-Covid “normal” within two years.
“I’ve said November 2021,” predicts Zeke Emanuel, former Obama adviser and chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania. “I think you’ll have enough herd immunity [in the U.S.] that we’ll have an unremitting decline.” Herd immunity is the point at which so many people are immune that the virus can no longer spread widely.
Florian Krammer, professor of vaccinology at the Icahn School of Medicine at Mount Sinai, put it this way: “What I think is going to happen at some point in [20]21 is the virus is basically morphing from a real spread into something that’s in the way and causes some low numbers of cases and probably very low numbers of deaths.”
The precise timing, of course, is uncertain—an elusive future that rests on a series of known unknowns, things like how many people continue to wear masks and social distance and whether rapid Covid-19 tests become widely available and properly deployed. Much will depend on how effective the vaccines are, how many people refuse to get inoculated and how many people forget to get their second dose if the vaccine requires two (yes, that is a significant concern). And then there’s what epidemiologist Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, calls “the trillion-dollar word of the day with this disease”: immunity. How long, on average, will immunity from natural infection and from the vaccine last?
“We can get [to herd immunity] with vaccination and clinical disease,” he says. “The question is how long can we stay there. Meaning, if we get to, say, 75 or 80 percent immune projection, would it stay that way if we didn’t do anything else?”
Perhaps that’s the most important thing to understand about the pandemic right now: Though experts can make their best guesses, there is no certainty about Covid-19’s future. “If this were an influenza pandemic, I would feel confident telling you how it would end,” says Osterholm. “But this coronavirus keeps throwing us curve balls day after day.”
This kind of unpredictability is why Sarah Cobey, an epidemiologist at the University of Chicago, chose her field in the first place: “One of the reasons I wanted to study infectious disease dynamics is that they can be really unintuitive. They can be mathematically very predictable, but they can always be unintuitive.”
Before the vaccine: ‘Masks and distance’
The pandemic is far from over. It’s not even in decline. Cases of Covid-19 are on the rise in more than 19 states, and in just one day this week, the U.S. saw more than 40,000 new cases and more than 1,000 deaths.
Experts don’t expect those numbers to improve much as people move indoors for the fall and winter. Harvard epidemiologist Michael Mina sees norms shifting as social distancing fatigue settles in: “Little by little there’s going to be fewer people wanting to sit outside, more people sitting inside,” he says. “And then people are going to say, ‘Well, you know, I was at dinner two nights ago and I was fine. I can go to this gathering of 30 people.’ Then ‘I can go to the gathering of 100 people.’ And it will probably be just kind of a slow … change of opinion about what the risks are.”

“Unfortunately, this is all occurring … at times that coronaviruses are very likely to potentially tick up due to seasonal effects,” he adds.
The expected surge underscores the idea that Americans are not going to achieve “normal” before a vaccine, not with this country’s outmatched testing system and total failure to contact trace. The key, then, to making sure that society finds some degree of normalcy in the meantime—meaning places like schools can stay open—continues to be “masks and distance,” says Emily Landon, chief infectious disease epidemiologist at University of Chicago Medicine. That means avoiding places like restaurants where you can’t wear your mask inside.
“Masks and distance really work,” she says.
Continued social distancing is far better than the alternative. Disease experts all warned against White House adviser Scott Atlas’ proposal to reopen the economy and reach herd immunity by letting natural infection tear through the population. Not only is the idea “a Russian roulette plan” that could lead to millions—millions—of deaths, says Landon, but the strategy might also be impossible, given that a sizeable chunk of the U.S. population is more likely to stay home than decide it’s OK to venture out to inevitably get infected. In that case, the United States would hover below the herd immunity threshold while the economy stays stagnant, achieving neither of Atlas’ goals.

There is another possibility, says Mina. There’s been recent buzz surrounding rapid Covid-19 antigen tests—cheap tools recently approved by the Food and Drug Administration that can deliver results within minutes. Some experts have questioned their utility, because they aren’t yet as accurate as more common lab-based tests. But Mina thinks that, if they’re produced on a massive scale and authorized for at-home use, rapid tests can help quell the pandemic in surge areas. The idea is that people would use them not as passports to enter crowded spaces and do things they wouldn’t ordinarily do, but as daily checks before they go about their normal business.
“They don’t have to catch everyone, because the messaging would have to be you do exactly what you’re going to do anyway. If the test is negative, you continue everything the same. But if the test is positive, then you definitely don’t go out,” he says. “We actually [can] use it as a tool to create herd effects so that you have enough people who are high transmitters not transmitting.”
The vaccine arrives: ‘I expect a little bit of chaos’
While many experts see value in strategies like vastly expanding testing, most agree that finding a working vaccine will be the biggest step on the road to normalcy.
The optimistic prediction that a vaccine will be ready for distribution by Election Day—put forth not only by Trump but also Pfizer CEO Albert Bourla—is looking increasingly unlikely. The two leaders in the U.S. race for the Covid-19 vaccine, Moderna and Pfizer, are still enrolling participants in their Phase III trials. In these trials, some participants receive a vaccine and the rest get a placebo, and then administrators wait to see who gets sick. U.S. presidents and CEOs can’t control the speed at which that happens. “It depends upon the frequency of [Covid exposure in] the neighborhood, how loose a person is” with masks and social distance, says Emanuel. Remember: The trial participants are still being told, like all Americans, to take precautions against infection.
An October vaccine authorization would require either a lot of participants to be exposed to Covid-19 in a short time, or a vaccine so effective that its power becomes apparent soon into the trial. But many experts doubt that the first-generation vaccines will be hypereffective. Plus, releasing a vaccine early carries the danger of missing a rare side effect, and drug companies in the world’s glaring spotlight will be reluctant to take that risk.
Nonetheless, given the urgency across the world, it’s probable that one or several approvals will happen at the end of the year or early next year. “Best-case scenario, we get a few vaccines that work by December,” says Landon. It could take longer. Larry Corey, who is in charge of coordinating the clinical trials of U.S. government-funded vaccines, has guessed the first U.S. Phase III results won’t be available until February.
Getting a vaccine out to the American people, of course, is a different problem—and a colossal one. Pharma companies and the U.S. government must produce, distribute and administer around 660 million doses of vaccine over the next year or so, because the vaccines furthest along in trials require two doses per person. Krammer says he expects “a little bit of chaos.”
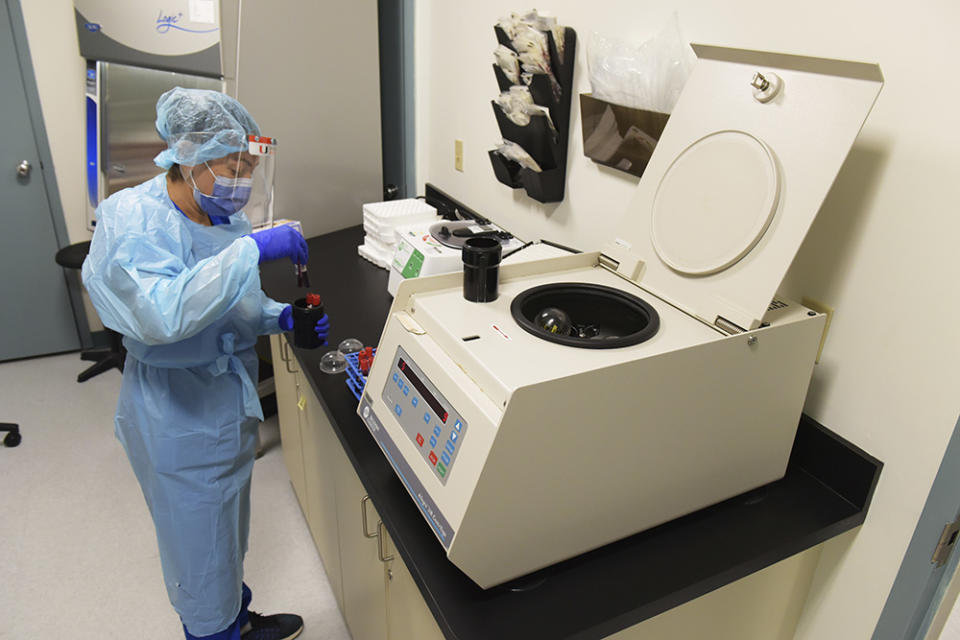
According to the U.S. government, hundreds of thousands of doses have already been made. But recent guidance from the Centers for Disease Control and Prevention indicates that only a few million doses of two leading vaccines—believed to be the Moderna and Pfizer candidates—will be available at first, to be given to essential workers and society’s most vulnerable.
Many experts, including the director of the CDC, predict that vaccines could be widely available as early as late spring or summer. But Emanuel believes that they’re underestimating just how difficult it will be to manufacture and distribute the doses at scale. In a report published by the Center for American Progress this summer, he and co-author Topher Spiro pointed out large gaps in the country’s vaccine setup, including potential shortages of production capacity, syringes and packaging.
And then there’s the problem of actual shot-in-arm delivery. Pfizer’s vaccine, for example, needs to be stored at minus 70 degrees Celsius. “No doctor’s office has negative 70,” says Emanuel. “You can’t do ‘the usual’—you know, this sort of hodgepodge we have of CVSes, Walmarts, … Walgreens, doctor’s offices, schools.” CDC guidance suggests states prepare to distribute doses at hospitals and mobile clinics.
Making sure that most Americans receive two doses of the same vaccine four weeks apart smoothly and efficiently will be a massive government operation—one that Emanuel thinks the country can pull off no earlier than November 2021—and that’s if you have “good management skills, good logistics,” he says. “If there is some element of optimism and not just realism, it’s in that. There is no evidence this administration has the capacity to manage that.”
After vaccination: ‘We have to wait to prove that it’s working’
It’s 2021, and you’ve just gotten your two doses. What happens next will largely depend on two factors: How effective the vaccine is and how many people get it.
The goal is for the vaccine to be effective and widespread enough for the U.S. population to reach the herd immunity threshold—the point at which, theoretically, Americans can safely take off their masks and attend large sporting events. A rough, back-of-the-envelope estimate for Covid-19 (derived from calculating the point at which each infected person, on average, infects less than one other person) is that society will reach herd immunity when around 60 percent to 70 percent of the population is immune.
Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, walked through the math: Roughly, “the formula would state that about two-thirds of the population would need to be vaccinated if [the vaccine] was 75 percent effective against shedding” (i.e., transmitting) the virus. If the vaccine is less effective than that, a greater percentage of the population needs to get vaccinated to close in on herd immunity. And vice versa.

Experts aren’t optimistic that these first-generation vaccines are going to be highly effective at preventing transmission. “The likelihood that we are hitting a home run in the first at bat is just very low,” says Michael Kinch, director of the Centers for Research Innovation in Biotechnology and Drug Discovery at Washington University in St. Louis.
Nor has the FDA set the bar very high: The agency indicated that any approved vaccine must prevent Covid-19 or decrease severity in at least 50 percent of those vaccinated, but that means more than 50 percent of the population could continue to transmit the disease.
Without a highly effective vaccine, the country needs relatively high vaccination rates. And yet a whopping two-thirds of Americans say they won’t get the vaccine when it’s first available—and a quarter say they’ll never get it. Many scientists fear that so many people are going to refuse to get both doses of a vaccine out of distrust or fear or just plain forgetfulness that America won’t reach a high level of protection, much less herd immunity.
“Apparently, these shots with Covid … they give you some fevers, some chills, you feel a little flu-like,” says Emanuel. “Well, how many Americans are coming back [to say], ‘Oh, I would like that again. I would like to feel like under the weather for a few days to get this vaccine.’ … What I worry about is we have a lot of people who are only partially immunized with one shot.”
There’s also the problem of even distribution. Some places like Boston, with its robust medical industry, might see very high vaccination rates, while states like Idaho and Colorado, with the lowest measles vaccination rate in the country, might end up with a lot of unprotected residents—and more disease. This is also a risk in Black communities in particular, where the coronavirus has taken an outsized toll but where distrust of the U.S. medical establishment runs high after decades of horrific experiments like the Tuskegee Syphilis Study.
“If you’re immunizing effectively above that immunity threshold, then it means that you can go back to business as usual,” says Cobey. “But that’s assuming … you’ve got the vaccine pretty evenly distributed in the population. And vaccines are almost never evenly distributed. Which is to say that you could easily have pockets like we’ve seen in Marin County and other places with measles [where] you can still get outbreaks.”

This isn’t a reason to panic. Any vaccine is going to be a big help in containing the pandemic. “Even if you don’t get herd immunity … the closer you get to it, the slower the virus spreads,” says Krammer, who expects many of the vaccines in development to work. “Fifty percent [effectiveness] is not that little.” But it won’t enable people to attend the theater or cozy up in their favorite dive bar right away. “I’m not sure people get that,” says Offit. “What worries me in this is that people would think, ‘Great. I’ve got the vaccine. I’m good. I can engage in high risk activity.’ And that would put us right back to where we were.”
Adds former CDC director Tom Frieden: “I think even with a vaccine, for the indefinite future, handshakes are out and masks are in.”
The key to figuring out what’s possible with a vaccine, Landon says, is patience. “You have to treat the vaccine the same as a masking policy. You make a policy that everybody has to wear masks and then some percentage of people actually do.” Similarly, “You give people a vaccine, and then some proportion of people will actually get the vaccine and some proportion of them will be protected.” Next, you wait to see whether the Covid-19 disease and death counts go down, which will take about two months after people receive their doses—a few weeks for people to develop immunity and then four to six weeks for that protection to appear in the numbers.
If rates are coming down, says Landon, “then you say, ‘OK, I think we can allow people to eat inside at restaurants.’ And then the rates stay low even though you invited people back to restaurants.”
Eventually, if the country doesn’t open too quickly, “we could find ourselves in a situation that China is in, that Taiwan is in, where we might still have limited little outbreaks here and there, but the majority of us can get back to most of the things that we used to do. We can have, you know, some parties … some gatherings.” She thinks we could get there by spring 2021 but that it will still take a couple of years to put the pandemic in the rear-view mirror.
It’s all about how many people in a given situation are likely to have Covid. Landon has been helping companies walk through the numbers as they consider whether to reopen their offices. If, for example, the positivity rate in a given population is 2.5 percent, as is true in many communities today, and “you have a company that has 100 people in it, two or three of them would have [Covid-19] on the day that you come back to work,” Landon explains. “And as soon as [companies] see that, they’re like, ‘Maybe we should keep working remotely if we can.’ But if you get it so that it’s only one in a thousand people who have Covid, having one hundred people together in a gathering place and putting masks on them means that no one’s going to get sick.”
This process is going to take much longer internationally. A coalition of international organizations—GAVI, the Center for Epidemic Preparedness and the WHO—are aiming to purchase and deploy 2 billion vaccines to the world’s most vulnerable in 2021. But Oxfam recently warned that 61 percent of the global population will not have a vaccine until at least 2022. Rich countries are not making equitable access easy: According to Oxfam, wealthy countries representing 13 percent of the world’s population have already reserved over half the supply of leading vaccine candidates.
Emanuel anticipates countries opening up international travel as they get and deploy vaccines, but that “it’s going to take a couple or three years to really get … a full return to pre-Covid normalcy” in international travel.
The years-long outlook: ‘They might get the sniffles’
The world will probably live with Covid-19 forever, even after inoculation. “I think a lot of people seem to think that vaccines automatically eradicate viruses,” says Rasmussen. “They don’t.” To date, only two viruses have ever been officially eradicated.
But many experts believe that, if vaccination rates are high enough, the Covid-19 of the future is going to be manageable, routine, just another virus that most Americans have some degree of immunity to. Some of that protection will come from natural infection and disease exposure; and some of it will come from vaccination.
“It’s very likely that in a vaccinated population, [Covid-19] would do very little damage,” says Krammer.

If protection from vaccines is found to wane within a year or so, as some people fear, Americans might end up getting a yearly Covid-19 booster with their flu shot, which is what Landon predicts. Or, vaccines could get more durable over time. “The way we’ve seen other vaccines historically has been that you get proof of concept … that one can work and then you’ll get gradual improvements,” says Kinch, who thinks we’ll see mediocre vaccines in the near future and a much better one in three to five years.
There’s also been a lot of worry about how long immunity from disease lasts; some Covid-19 victims have already gotten reinfected with the virus, in at least one case severely. While the media will always seize on the most unusual, most sensational medical cases, many infectious disease specialists believe that, even if a person’s immunity wanes after infection—as it does for other coronaviruses—future infections, on average, are probably going to be weaker than the first.
In fact, getting exposed to Covid-19 will be a crucial part of developing protection. “Eventually, you’ll have enough people who have … built up a little bit of immunity, whether that’s through vaccine or maybe you’ve been infected once. And then the next time you get exposed, it actually serves as a natural boosting event. It boosts your immunity instead of harms you,” says Mina.

“Let’s say somebody turns 60 in five years,” he games out. “They’re 55 years old now. They get a vaccine next year and maybe they get an exposure. By the time they’re 60, they might have had two or three exposures. And so they won’t be as at risk anymore when they’re 60 because they’ve now gained enough immune memory.”
Krammer envisions that in the long term, people will get vaccinated or infected when they’re kids, building up more immunity through revaccination and reexposure. “And by the time they are really in the high-risk group, which starts at 50, … they probably are not going to have a severe disease anymore, but they might get the sniffles,” he says.
At the same time, experts are crossing their fingers that treatments and therapies are going to get better, so that those few who do end up with severe cases are vastly more likely to live. An antiviral drug—which weakens a virus if you take it early enough—would be a game changer, says Landon, “but that’s some years away.” And it will be important for scientists to keep delivering new drugs and treatments. “Maybe remdesivir plus convalescent plasma plus two new drugs in the future and rolling someone on their stomach might do the job until … the virus naturally develops resistance to one of them and now you’ve got to substitute in a new drug,” says Kinch.
Some believe there will continue to be deaths, though, as there are with flu every year. But how many deaths might just depend on what society is willing to passively accept. Last year, in the United States, the flu sent 740,000 people to the hospital and killed 62,000. “We’re comfortable with that; we let that happen,” says Offit. “We go to sporting events, where it’s very possible we could catch the flu.” Conversely, many people in Japan wear masks during flu season.
Covid-19 will slowly but surely peter out, he says. “And then it’s a matter of what level of disease and death you’re comfortable with.”
Perhaps, faced with this calculation, large portions of American society will decide not to follow the inexorable track back to “normal.” Perhaps masks will become the norm in winter, when coronaviruses spread more readily, and handshakes won’t return.
“I think there’s going to be a fundamental fear,” says Kinch. “My grandparents lived through the Depression. And for the rest of their lives, even when they had money and some degree of financial security, they to a degree acted like they were living through the Depression.”
“And that’s not meant [to be] gloom and doom,” he adds. “The new normal will be fine, and we’ll get through it just fine. But I don’t think we’ll go back to January in my lifetime.”

