Pandemic sent Delaware Public Health District costs, staffing hours skyrocketing
The economic havoc caused by the COVID-19 coronavirus pandemic extended to the Delaware Public Health District and the Ohio Department of Health, as each experienced spiraling costs while expanding operations to battle the pandemic.
As of March 31, the health district's COVID expenses not covered by grants totaled $698,634, said district commissioner Shelia Hiddleson. That amount was paid primarily with levy funds from the district's general-revenue fund, she said.
"The COVID-19 pandemic represented the longest sustained threat to Ohio’s public health in more than 100 years," said ODH spokesman Ken Gordon. "It required an unprecedented commitment of personnel, resources and funding."
As of March 31, Ohio had spent $1.01 billion in COVID-related funding from the federal government, which Gordon called Ohio's primary funding source against the pandemic.
In late 2019, the Delaware health district had 73 staffers, Hiddleson said, and its disease-control response team had six people.
At times during the pandemic, the district's workforce increased to more than 90, including contracted workers, she said.
The health district closed its offices during the statewide lockdown but maintained its services, Hiddleson said.
"Staff worked up to 12 hours per day, seven days per week for many months. This began in April of 2020 ... and the seven days per week did not end until after May 2021," she said.
As the pandemic gathered steam, she said, the district employed up to 10 clinical-services aides at a time to assist with contact tracing and up to four contracted data-entry assistants.
The district had to develop forms to meet reporting requirements, she said, and depending on the tasks given to the new people, training per person ranged from 16 to 40 hours.
By the end of 2021, the overall staff had dropped to 72 people, she said.
Preparedness before COVID hit Ohio
In August 2019 – still months before the coronavirus was identified in China – Hiddleson had told ThisWeek one of the health district's routine tasks was to prepare detailed contingency plans in case of communicable-disease outbreaks.
Those plans were put into action in response to COVID in January 2020, before Ohio had a confirmed case, she said April 19.
That happened because of an alert system employed by the Centers for Disease Control and Prevention, designed to spot emerging contagious diseases, even outside the United States, she said.
As part of the predetermined plan, the health district was prepared to interview and if needed quarantine those returning to the county from an area experiencing a contagious outbreak, she said.
"This wasn't new. This has always happened. But I never imagined the magnitude with COVID," she said.
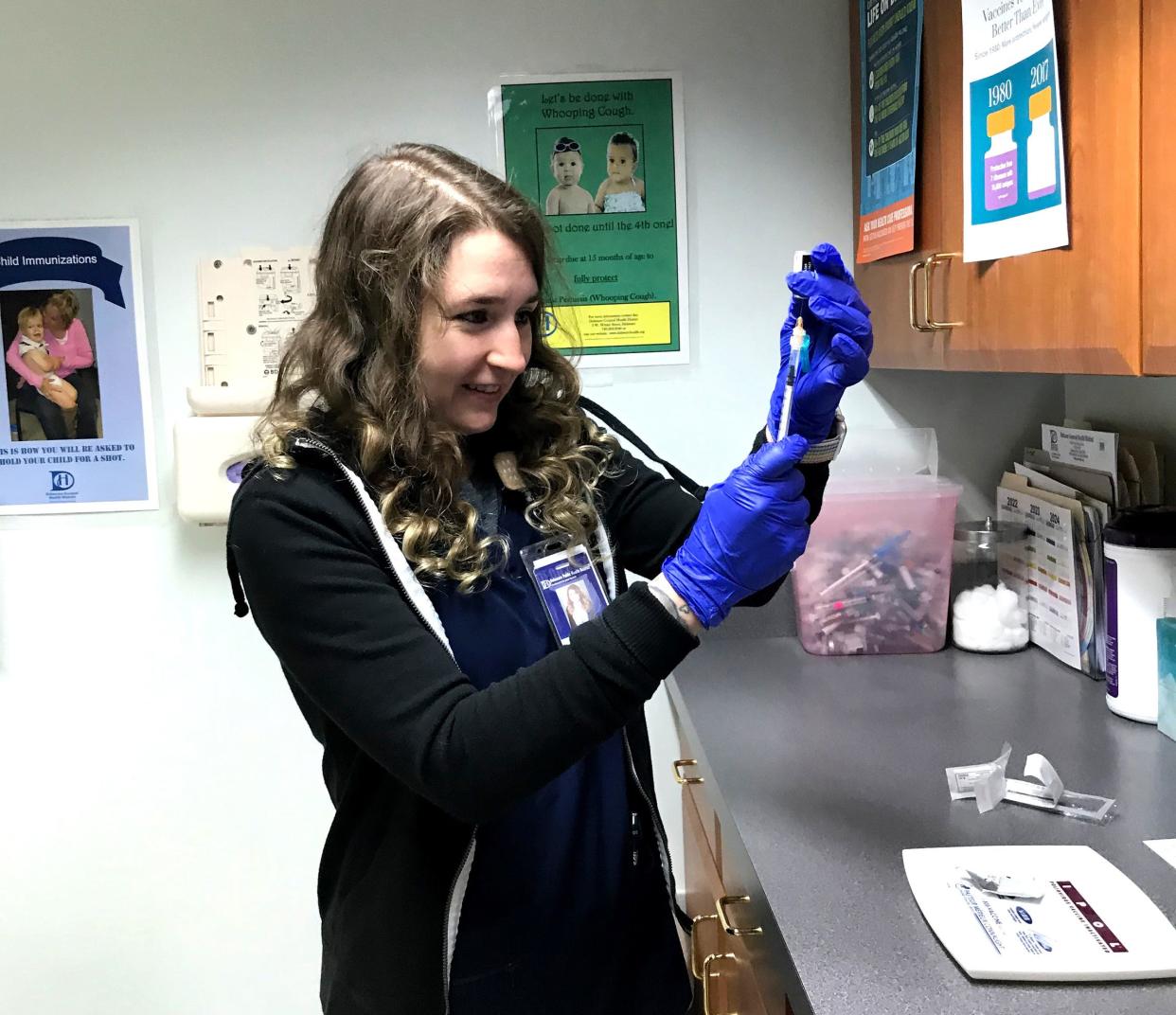
As of April 19, the health district had administered more than 30,000 COVID vaccinations, Hiddleson said.
Its vaccination program was started in December 2020 and has involved over 3,300 hours donated by 275 volunteers, she said.
Delaware County has a high vaccination rate, Hiddleson said, including nearly 90% of its elderly residents vaccinated.
Health district records show that in the year preceding March 2022, 69% of Delaware County residents hospitalized with COVID were unvaccinated and 70% who died after being diagnosed with COVID were unvaccinated.
From January to March 2022, 82% of its residents hospitalized with COVID were unvaccinated and 53% who died after being diagnosed with COVID were unvaccinated, the records show.
Both Hiddleson and Gordon said the response to the pandemic has not stopped but is operating at a smaller scale because of the lower number of new cases.
The ODH website said that as of April 14, 4,808 new suspected COVID cases were reported statewide in the preceding week, an average of more than 680 a day.
Delaware County, ODH keeping up with routine tasks
The health district's routine services also continued during the pandemic, Hiddleson said.
Environmental-health programs and WIC – the nutrition program for women, infants and children – continued with only minor interruptions, she said.
In July 2021, many staff were returned to normal duties, but the surge later in the year required many to return to COVID-related efforts, she said.
Gordon said Ohio's COVID response was coordinated by the governor’s office and reached across state government.
"ODH partnered with the departments of Aging, Developmental Disabilities, Medicaid, Mental Health and Addiction Services, Public Safety, Veterans Services, Administrative Services, the Office of Budget Management, Ohio EPA, Pharmacy Board and Bureau of Workers Compensation, among others," he said.
The federal grant money has been used for a variety of needs during the pandemic, Gordon said.
"For example, to enter into contracts to help with staffing, such as with ProLink to provide nursing staff to local health departments or (consultants) PCG (Public Consulting Group), which had more than 600 contact tracers active during the peak surge times."
ODH has purchased millions of COVID-19 tests and made them available to community partners statewide, he said.
"The department also sent millions of dollars to local health departments to help them in their efforts."
In addition, the department has spent funds to implement and grow its wastewater monitoring network, which collects wastewater from 74 treatment plants, Gordon said. The water is tested for levels of coronavirus, and the system serves as an effective early-warning system if viral levels increase, he said.
ODH staff manned a COVID-19 information center and reported cases, hospitalizations and deaths daily from March 2020 to March 2022, he said. That effort required an unprecedented level of work, encompassing evenings, weekends and holidays, Gordon said.
Throughout the pandemic, Hiddleson said, the health district’s staff have worked to do everything it could for the community.
Partners' and volunteers’ efforts appreciated
The health district's community partners, including law enforcement, EMS units, elected officials, nonprofit organizations and government public-information officers, reached out to the health district and helped disseminate factual information to the community, she said.
She also thanked volunteers who stood outside in freezing weather when the health district held its first drive-thru vaccination clinics in the winter.
In early February 2022, all health district staff returned to normal duties, with the exception of the disease-control response team, she said.
That team, with the assistance of about four clinical-services aides and two contracted data-entry assistants, continues to respond to COVID and complete all case-management and follow-up documentation, she said April 19.
Amid all else, the pandemic disrupted the health district's plan to build a new headquarters at 470 S. Sandusky St. in Delaware, Hiddleson said.
The health district in 2019 announced the plan to build the structure, predicting it would open in 2021.
"COVID has delayed it immensely," she said.
The pandemic-related lockdown created the first delay, she said, and supply-chain problems still plague the project.
The project's contractor has had problems finding enough workers, she said, and at least one subcontractor went bankrupt.
editorial@thisweeknews.com
@ThisWeekNews
This article originally appeared on ThisWeek: COVID sent Delaware Public Health District costs, hours skyrocketing

