I Was Part of Moderna’s COVID-19 Vaccine Trial. Here’s What the Side Effects Were Like.

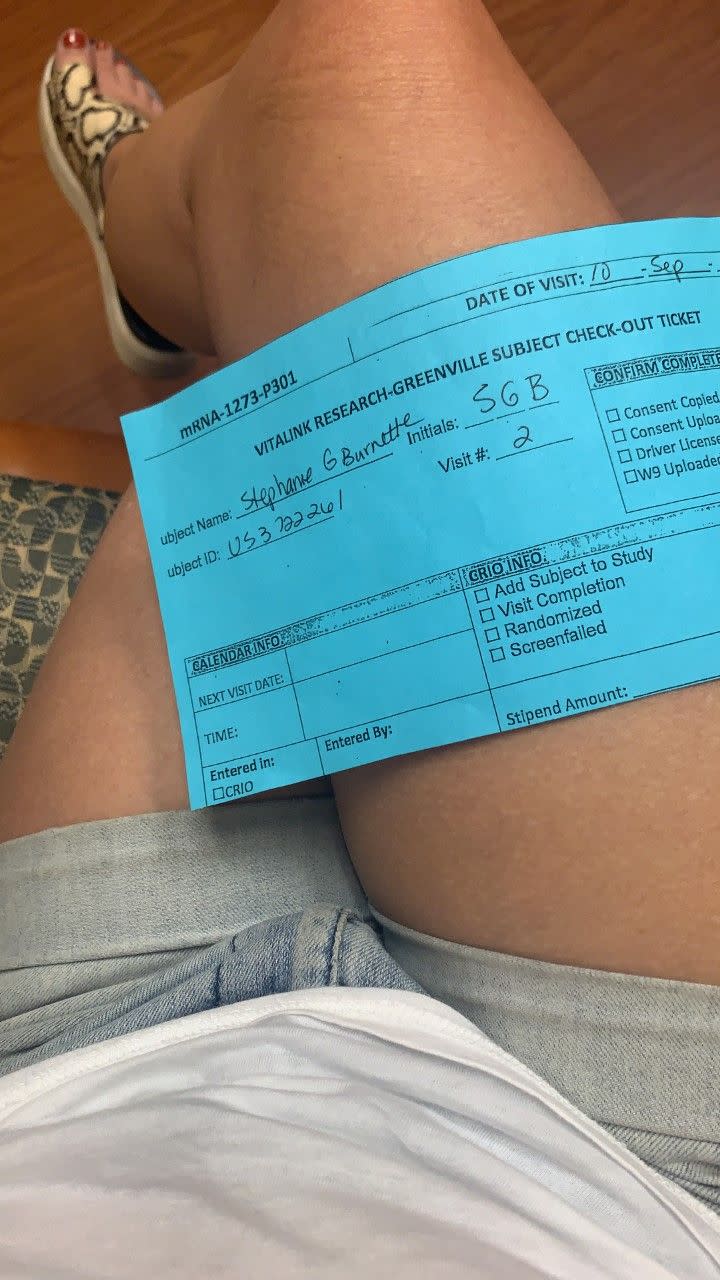
In December 2020, the Food and Drug Administration granted an emergency use authorization for the Pfizer and Moderna COVID-19 vaccines. Shortly after, Americans started to line up for their first dose. For this to happen, volunteers had to take part in clinical trials: This is the story of Stephanie Burnette, a 47-year-old married mother of two from Greenville, South Carolina, who participated in the Moderna trial.
My grandmother lived to be 104. As a child, I’d touch her scar from the smallpox vaccine, an oval of needle pricks on her upper arm while she laughed at my morbid curiosity. And here I am, a century later, in the midst of a global pandemic, rolling up my sleeve to help find a stop.
I was part of Moderna’s phase 3 COVID-19 vaccine clinical trial. When a friend sent me a link to sign up, I jumped, without hesitation, at the chance to be part of history—and science. Besides being an overall curious cat, I was fascinated with what I’d been reading about the scientific community’s approach to this particular vaccine’s development; while many vaccines, such as the flu shot, actually inject you with a small piece of the virus itself, in this instance, scientists said they’d found a way to manipulate messenger RNA to fight off COVID-19. Now, I’m sharing my story in the hopes that it will help ease the fears of those still on the fence about getting vaccinated.
Deciding to volunteer
At the end of July, I submitted an online form expressing my interest in being part of this groundbreaking scientific study. The very next day, I got a call asking me to verify simple information like my name, age, was I pregnant, and to ask if I was involved in any other trials.
Over the next couple weeks, I spent two more phone calls sharing my medical history in greater detail: I was asked what medications and supplements I take, as well as whether or not I had any of the health issues that are thought to make COVID-19 particularly dangerous, such as being actively treated for heart disease, having asthma, or smoking. But I’m a healthy 47-year-old, so no red flags “disqualified” me from participating—and one day at the end of August, just three weeks after I’d applied, I was off to the lab.
Once at the research lab, located in Greenville, South Carolina, I was given a 20-page contract to read and sign; it described the trial in great detail and explained that my medical info and blood draws would be used in other ways even after the study concluded. That gave me my only moment of pause, since it was a reminder that it’d be used for reasons beyond diagnosing or helping me specifically—but the document also clearly stated that I could leave the study at any time. That was the push I needed to scribble down that last set of initials: I was not contractually bound to continue if I started feeling weird or second-guessing things. Plus, I reminded myself, if millions of people could be helped by an effective COVID-19 vaccine, then I was fully on board.
The first shot
Once I was officially one of the 30,000 adults who were willingly turning their bodies over to Moderna for science—that’s the number of volunteers needed to participate in each vaccine trial to help prove that it’s safe and effective—a nurse took my vitals. I was swabbed for coronavirus up both nostrils, and had eight vials of blood extracted from my right arm.
Then, the moment of truth: The nurse released a numbered syringe from a Mission Impossible-looking lockbox and injected it into my left shoulder. Since the Moderna vaccine trial was 50/50 drug-to-placebo, I had no clue if I was receiving the real deal or a saline-filled syringe, but I was excited anyhow. It was the smallest, slightest prick. Easier than a flu shot. Barely a mosquito bite. I sat in a recliner with a mask on for 30 minutes while they closely monitored my temperature and kept an eye out for any allergic reaction. Then, just like that, it was over, and I left.
When I got home, it was life as usual. I’m a freelance writer/editor, so I settled in to finish writing up a story about how to cook with pomegranates. As I admired the pretty photos that were set to accompany it, I noticed my arm felt a bit tender, similar to how it feels when you get a tetanus shot. It stayed that way for a few days, over which I also had periods of feeling dog-tired. But as we now know is the case, that first shot is unlikely to trigger any overwhelming discomfort, and I didn’t experience any other noticeable side effects. For the first seven days following my first injection, I logged my temperature and any symptoms into a secure app, and a nurse called to check up on me a few times. I felt fine, but that early tenderness and fatigue set off a volley of thoughts that would pop in and out of my brain until my next shot: Did I get it? Is that what those symptoms meant? I can’t wait to find out.
Life after the second dose
Twenty-seven days later, in mid-September, it was time for my second shot. It was the same drill—tiny, nearly painless prick—but this time, the after effects were much different when I got home from the lab. My arm ached within the hour, and I was so sleepy I knocked out by 9 p.m., only to be awoken a few hours later by a serious case of the chills. For the next 30 hours, I rarely got out of bed. I maintained a low-grade fever and rode a merry-go-round of sweats, chills, body aches, and extreme fatigue. I toggled over-the-counter meds to help manage my fever and bodily discomfort, and I tracked my symptoms in the app. But amidst my misery, I felt something else: elation. My body was responding to something other than a saline placebo. I had received the actual Moderna vaccine, and I couldn’t have been happier.
These side effects are totally expected and “basically show that the immune system is being primed,” Richard Watkins, M.D., an infectious disease and professor of internal medicine at the Northeast Ohio Medical University recently told Prevention. When you get the vaccine, your body is learning to mount a response to SARs-CoV-2, the novel coronavirus, which can lead to short-term symptoms like a fever. (The vaccine doesn’t contain the actual virus, so it can’t give you COVID-19.)
When I awoke on the morning of day three, I was happily shocked—my symptoms were nowhere in sight; they’d disappeared like a light. It was the craziest thing. I went from living in bed to walking with my husband to one of our favorite neighborhood spots for a mimosa and hot chicken biscuit outdoor brunch. I felt normal, not a tinge of wonkiness remained.

I returned to the clinic to offer up more blood a month later, and there will be more phone calls and in-person visits over the next two years to help determine how long the vaccine can provide protection. My blood will help uncover this, in part, by measuring my antibody load over time.
I am a labeled, numbered lab rat. And that is fine by me. Scientists are still trying to determine whether this will prevent me from actually contracting the coronavirus itself, or if it just makes my body better able to fight it off without feeling sick (that’s why medical experts are urging people to still wear a mask even once they’ve been vaccinated). But I still feel hope—and that’s a small bit of comfort in this ever-changing world.
Go here to join Prevention Premium (our best value, all-access plan), subscribe to the magazine, or get digital-only access.
FOLLOW PREVENTION ON INSTAGRAM
You Might Also Like

