Plasma Files: How a device shelved for health reasons in France remained in use in U.S.
Donating plasma has long been a way of making money, especially among people on the financial margins. Unlike with blood, plasma donors are paid cash and can donate twice a week.
Plasma, the liquid portion of blood, is the key ingredient in medicines produced to treat a number of rare health conditions, including the blood-clotting disorder hemophilia. And since the onset of the COVID-19 pandemic, plasma has taken on new importance because patients who have recovered carry antibodies in their plasma that some scientists believe can be used to help others stave off the effects of the illness.
One of the most commonly used devices to collect plasma — including from recovered COVID-19 patients — was effectively banned in France in 2018 because of concerns about the presence of mysterious particles in the collection materials. The machine still isn’t in use there.
But the the machines, manufactured by a Massachusetts-based company called Haemonetics, remain in widespread use in the rest of the world, including the United States.
And an investigation by an international consortium of seven news organizations, including the Miami Herald and McClatchy, in conjunction with The Signals Network, has found that the particle problem wasn’t limited to France and has continued to be flagged at plasma collection centers and other healthcare facilities.
According to hundreds of new documents provided by whistleblowers to the media partners, there have been more than 150 customer reports indicating the presence of particles by plasma collection centers and other healthcare facilities in the United States between 2005 and 2019 associated with Haemonetics machines. That’s far more than in any other country in the documents, which also show that particles were reported in more than two dozen locales, including Germany, China, Japan, Taiwan, Canada, Sweden, Netherlands, United Kingdom and Australia. The company acknowledged that it has received more than 2,000 customer reports indicating the presence of particles related to plasma collection procedures in the past 15 years, but said such complaints represent .0006% of the more than 360 million plasma collection procedures that have been conducted using the machines in that time period.
It isn’t clear exactly what’s causing the particles to appear, but some of them have been found to contain trace elements of various metals, including zinc. Experts say metal particles have no place in the plasma collection kits, which are designed to be sterile and single-use, and could pose long-term health risks to donors.

Haemonetics describes its machines as the most popular devices used at plasma collection centers, the facilities where donors are paid to give plasma. CSL Plasma, the largest of those plasma collection companies, says it uses Haemonetics PCS2 machines in all of its more than 250 U.S. facilities. CSL Plasma, which is headquartered in Boca Raton, denied that particles have been found in any of its collection centers.
Haemonetics has publicly said that the particle problem posed a “neglible” risk to donors, but internal records show that Haemonetics employees were more concerned about the potential health risk they posed. And the ban in France ultimately came about after multiple former Haemonetics employees came forward to health authorities to flag the problem.
In the United States, there has also been another issue: A spike in the deaths of donors who donated plasma using a PCS2 machine in the past three years. While there’s no indication the deaths are connected to the particle problem, it raises further concerns about whether the millions of donations made each year with the devices are putting donors at risk.
Problems on the rise
Issues with the machines are rare, but the potential risk that the particles could pose to donors is what led France to shelve the only disposable collection kit that was used at the time with PCS2 as authorities determined what was in the particles and how dangerous they were. The machine remains out of use in the country.
The particles pose the greatest risk to donors, because the rest of the blood is returned to donors after the plasma has been removed, which could allow the particles to enter a donor’s bloodstream. Most of the plasma collected with the PCS2 is turned into medicine, and undergoes a purification process before it is ever given to a recipient.
Haemonetics said in a lengthy statement that its devices have a long track record of safe use.
“Haemonetics’ blood and plasma collection devices and disposables have been used for decades worldwide to safely and effectively collect plasma, platelets and other blood components. In the past 15 years, our products have been used safely in more than 360 million plasma collection procedures globally. We operate in 50 countries and comply with all local laws and regulations covering our operations and products. The safety of Haemonetics’ products for donors, patients and users has been and will remain our top priority. The global need for plasma and plasma-derived medicines is well-documented and it is important that donors and patients alike understand the long track record of safety around blood component collections.”
We want to hear from you
If you work in the tech industry and believe in good faith the public is being harmed, exploited or misled by powerful corporations with access to big data, please let us know.
None of the U.S. particle cases are listed in the Food and Drug Administration’s database of medical device reports (MDRs), which manufacturers are required to submit within 30 days of learning that one of their devices is connected to a death, illness or malfunction that could potentially cause illness or death.
Haemonetics has maintained that the particles found in their devices pose a “neglible” risk to donors and stresses that they have been found to be non-toxic.
But Haemonetics has reported to the FDA a sharp increase in deaths involving the PCS2 device over the past three years — with 35 deaths reported after use of the machine since 2018, the majority of which were reported in 2020, much later than they actually occurred.
Haemonetics chalked up the late reports to a technical error.
“During 2018 and 2019 a number MDR reports of were evaluated appropriately and filed on time through Webtrader [the FDA MDR portal], but recorded as being late because of a technical error,” the company said. “Haemonetics self-identified the error, proactively informed the FDA and rectified it.”
Haemonetics reported only five deaths connected to the PCS2 between 2010 and 2017. All told, the PCS2 and a newer model, the NEXSYS PCS, have been connected with more than half of the 82 deaths reported after use of such devices in the past decade, according to FDA data.
The reports don’t indicate where the deaths occurred and whether the machine “caused or contributed” to the death, and Haemonetics classified seven of the deaths reported as not being an “apparent adverse event.”
But the reports do frequently provide information about the circumstances under which a donor died. Roughly one-third of the PCS2 reports in the past three years mentioned heart attacks or other heart-related conditions.
While the donation process doesn’t typically lead to heart issues, Jeffrey Winters, the vice chair of the division of transfusion medicine at the Mayo Clinic, said a donation could exacerbate an underlying heart condition. Blood and plasma donors typically receive a health screening before they are allowed to donate, he said.
“We ask people when they come in to donate, are you under a doctor’s care for anything?” Winters said.
He said some patients might not be aware, or might not accurately represent, their underlying health conditions.
“I see that even in our own donor center here, where sometimes people will minimize things that are happening in their life with their health,” he said.
Winters and other experts say the sudden increase in reported deaths needs to be examined.
“That should definitely be a signal that the FDA would investigate,” said Madris Tomes, a former FDA subject matter expert on adverse events for medical devices and founder of the medical consulting company Device Events. “The FDA needs to make it a priority to determine if this is serious enough to recommend a recall or issue a public statement. Those who donate plasma should not be put at risk under any circumstances.”
Haemonetics said that the increased number in reported deaths during the past three years was the result of a change in policy.
“[I]n 2018, out of an abundance of caution, Haemonetics voluntarily changed its MDR reporting approach to be more conservative and to align with the reporting practices of our plasma customers,” the company said. “This means Haemonetics began filing a MDR/vigilance report for any plasma donor fatalities reported to us, regardless of whether the device may have caused or contributed to death or serious injury.”
The FDA didn’t answer specific questions about the particles or about the recent spike in deaths reported by Haemonetics, but provided the following statement:
“The FDA is responsible for ensuring the safety of the nation’s supply of blood and blood components and is committed to helping ensure the health and safety of donors and patients. The agency’s regulatory framework and reporting requirements, along with robust partnerships with regulatory partners around the globe, help the FDA identify and evaluate technical issues related to the safety of the blood supply and work to mitigate any potential adverse events. Among the millions of transfusions and donations annually in the U.S., associated adverse events, including fatalities, remain extremely low.”
Blood money
Haemonetics was founded in 1971 by Boston engineer Jack Latham, who pioneered the concept of the single-use collection kit, inventing a disposable plastic centrifuge to separate the different components of blood. It became known as the Latham Bowl. The machines take in blood from patients and then spin the blood at a high speed in the disposable bowl to separate out the plasma from the rest of the blood. The plasma is transferred into a collection bag while the remainder of the blood, along with a saline solution and anticoagulant, to prevent clotting, is then returned to the donor through a filter that blocks anything larger than 170 microns, roughly equivalent to three follicles of human hair.
The French ban didn’t diminish investors’ confidence in the publicly traded company, which is valued at roughly $4.3 billion. It was one of the best performing stocks in 2018 and its stock closed at a record high $138.52 on Aug. 16, 2019, nearly one year after the French ban took effect. The company’s stock price has slid in 2020, but that has more to do with concerns about the impact of coronavirus on demand for its products than on safety concerns.
Plasma is big business across the globe — with the market for plasma proteins valued at more than $22 billion in 2018. Plasma is the raw product for a number of medicines used to treat rare illnesses, such as the blood-clotting disorder hemophilia and several autoimmune disorders. Those medications require a lot of plasma to manufacture — the industry says it needs 1,200 donations a year to produce enough medicine to treat one patient suffering from hemophilia. And the industry has stepped up to meet the demand in recent years. There are now more than 850 collection centers across the country and the number of annual donations has doubled in the past decade, to more than 53 million donations in 2019.
The plasma industry represent the biggest chunk of Haemonetics’ business, with equipment, software and support for plasma collection companies representing just under half of Haemonetics’ total revenue, according to its most recent annual report. Haemonetics’ two biggest plasma clients, CSL Plasma and Grifols, are also the two biggest plasma- collection companies in the world.
Plasma donors are paid for their time. Grifols, which operates under a variety of brand names including Biomat USA, Inc, Talecris Plasma Resources, Inc. and Biotest Plasma Center, Inc, advertises that donors make an average of $200 a month for donating plasma. Because plasma donors in the United States can donate more than twice as often as donors in Europe, plasma collection centers frequently offer additional bonuses to incentivize repeat donations or lure in first-time donors. Globally, roughly 60 percent of the plasma used to produce plasma-derived medicines comes from North America. The centers tend to be in poorer areas, and donating plasma has increasingly become a survival strategy for many Americans struggling to get by.
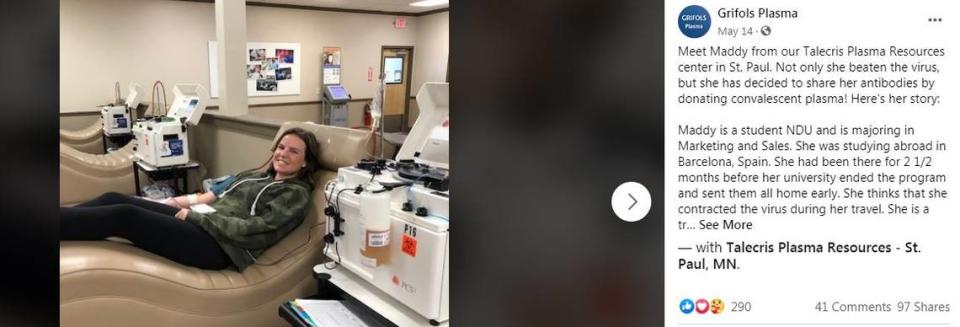
The Miami Herald reached out to more than a dozen plasma collection facilities across Florida and confirmed that the Haemonetics PCS2 is in use in several of them and being used in some facilities to collect so-called convalescent plasma from donors who recovered from COVID-19 to be used to treat patients suffering from the virus. A social media post by Grifols promoting COVID-19 convalescent plasma shows a recovered COVID-19 patient donating plasma with a Haemonetics device.
The potential health risks from the particles would be greatest to donors and not recipients, since most plasma collected by for-profit collection centers ultimately goes through a process referred to as fractionation, by which plasma is broken down into its various components and then purified before being manufactured into various therapeutic medicines. Much of the COVID-19 convalescent plasma, for example, is destined for use in hyper-immune globulin, which would be given to COVID-19 patients to help boost their immune response to the disease.
Metal mystery
While it’s unclear exactly what is causing the particles to appear in Haemonetics machines, one crucial difference between its devices and those produced by its top competitors is that the disposable bowl in the PCS2 contains two metal rings that are part of a swivel joint that rapidly spins the bowl to separate plasma from the rest of the blood. That’s part of Haemonetics’ competitive advantage, since it helps speed up the collection process, but it’s also thought to be connected to the presence of the particles.. Haemonetics’ primary competitors, German company Fresenius Kabi and Japanese company Terumo BCT, don’t have metal joints that come in contact with each other in their disposable collection materials.
A scientific investigation commissioned by French health authorities before the 2018 ban determined that the particles that led to the ban in France, found in both the collection bags and the centrifuge bowl, contained small quantities of zinc and aluminum, among other components.
“It’s highly unusual to find metal particles inside any of these single-use kits,” said Joseph Roig, an expert on plasma and blood collection devices, who worked for nearly 20 years at Haemonetics’ rival Terumo BCT, with many of those years on the scientific support team.
Roig said it’s not uncommon for small plastic particles to make their way into collection bags and tubes because the materials in the equipment are largely plastic.
“I never heard about non-plastic particles,” he said.


Foreign material
When the machine was banned in France in 2018, it wasn’t the first time mysterious particles had been found in the Haemonetics centrifuge bowl or collection bags.
Internal documents provided by whistleblowers to McClatchy/Miami Herald and media partners show that company officials were worried about the health risks of the particles after they were discovered in bags of plasma that were being transfused into patients by the Dutch blood bank Sanquin NL.
A Haemonetics sales and application specialist sent a panicked e-mail on May 27, 2011.
“At the moment I do not know whom to turn and I’m looking for some advice and counsel from people I know and trust,” he wrote. “Monday I will need to come with an explanation to one of our customers, I need to know what to communicate to minimize damage now [that] a patient is involved.”
He expressed concern because of “increasing reports” of such incidents.
“I really need advice,” he wrote. “Do we know 100% sure what kind of material this is floating in our plasma?”
The company investigated and disclosed the issue to customers later that year, describing the risk to donors as “negligible.”
In a September 2011 letter, the company’s chief medical officer, Mark Popovsky, notified customers that “particulate” had been generated during collection using a high-separation collection bowl in several instances in Europe. Popovsky said the particles were primarily proteins from the blood, but also included some “carbon particulate.” He wrote that tests of the particles showed them to be non-toxic and wrote that the company believed a change to the manufacturing process of the bowl had likely contributed to the problem.
He described the incidence of such particles as rare — with 29 reports of the problem since October 2010 — and said the risk to donors was negligible, since larger particles generated during collection wouldn’t pass through the 170 micron filter when the remainder of the blood is returned to a donor. The company advised that the high-separation bowl, which was faster than the standard bowl, was safe for collecting plasma that would ultimately be manufactured into medicine, but advised against using it to collect plasma for transfusion directly into a patient.
But though the company adjusted the manufacturing process to address the problem, the issue persisted.
The following year, Sanquin NL discovered black particles again in a plasma bag in a machine that was supposedly fixed.
“This is timely information to let you know that we received a brief message from Sanquin about a black particle that is found in plasma using a ‘corrected’ device,” wrote a senior sales manager in the donor division, in an e-mail dated Nov. 22 2012.
Haemonetics would again examine the particles. A report by the company’s senior scientist, Yair Egozy, determined that the majority of the material was biological in nature, likely from blood, but that time some of the samples also contained zinc, nickel and copper. Egozy couldn’t definitively determine where the metallic components had come from. The metal ring in the bowl contained zinc, but none of the other metals.
“They could have started with small fragments of carbon ring material, covered with organic matter that made them shiny, or they could have been external contaminants, which were introduced during assembly of the harness, or, more likely, during the processing and analysis of the samples,” Egozy wrote.
The particles didn’t stop appearing, though. And eventually two Haemonetics employees in France, Alexandre Berthelot, the former Haemonetics managing director for France, and Jean-Phillipp Urrecho, a former Haemonetics senior technician, went public as whistleblowers with concerns about the safety of the company’s machines, after unsuccessfully raising the concerns internally. Starting in late 2015, they began sending letters to various French health agencies flagging issues with the machines.
They were joined in their efforts by another whistleblower, Guylain Cabantous a union official at the public organization that oversees blood and plasma donation in France. And in February 2017, the French publication Mediapart published an investigation about Haemonetics, which mentioned the particle issue, along with other health concerns raised by the whistleblowers. Around the same time, a French scientific committee began to investigate Berthelot and Urrecho’s complaints and found that the machine produced black particles containing zinc and aluminum. The committee found that a machine produced by a rival company also posed a risk for generating particles, but characterized the risk of particles as greatest with Haemonetics devices because of its rotating metal joints.
Because of the discrepancies in the metals found in the samples from the Dutch company and those assessed by the French authorities, it’s difficult to reach a definitive conclusion about the source of the particles, or the risk to donors or recipients.
“With the available data, a toxicological assessment of the risk to patients is not possible,” Dirk Walter a particle expert at the University of Giessen in Germany, told the Miami Herald’s reporting partners. “This is not ... to absolve the company … it’s bad not knowing all this.”
Winters, of the Mayo Clinic, said that he thought it was unlikely the smaller particles were causing short-term harm, such as an immune reaction or obstruction of blood flow, because it would have likely led to a spike in such incidents that would have drawn attention, but he said they could still prove harmful.
“You would have to be concerned, could that cause long-term health problems to people,” he said.
Haemonetics said it has designed its collection kits to be “biocompatible” so that they pose no harm to people.
“We have extensively tested both the components of the kits and the finished medical devices to ensure they are safe and non-toxic for humans,” the company said.
But Rainer Blasczyk, head of the Institute for Transfusion Medicine and Transplant Engineering at Hanover Medical School, said the presence of particles should not be tolerated in plasma donations.
“Something like this must not happen at all,” he said. “Foreign material of any kind must not enter the body through a plasma donation.”

