Putting the 'home' in long-term care means big changes, community buy-in

When Barry Sheehan thinks about his care at the Osgoode Care Centre in south Ottawa, his mind often turns to the food.
"They promised me that I would have a lobster roll," Sheehan said with a chuckle. "I thought they were joking!"
Originally from New Brunswick, the 81-year-old moved into Osgoode Care partly to be closer to his daughter Katie Cote and her family. But Sheehan still misses the Maritimes.
"It was fun and good to see all the people who had never had a lobster roll enjoy it," he said.
That kind of attention to the life people had before moving into the independent, non-profit home is part of a shift for the 100-bed care facility, which has since 2016 been incorporating the Eden Alternative model into its program.
Eden Alternative, one of the "person-centred" approaches to care that first emerged in the United States in the 1980s, focuses on fighting the "three plagues" that affect long-term care residents: loneliness, helplessness and boredom.
Part of that involves encouraging greater connection between staff and residents, and creating more intimate spaces that feel like home.
The Sherbrooke Community Centre in Saskatchewan has been a registered Eden Care Community since 1999, while Nova Scotia started a provincewide plan to create a care model mimicking familial care in 2009.
While the pandemic sharpened the focus on long-term care, the sector has had to continue implementing these changes even as attention shifted.
Most recently, the City of Toronto launched a pilot program, mostly funded by the province, for its municipally run long-term care homes to develop their own models of care. Quebec is developing its own care model, drawing on the larger culture change movement.
But change can be more expensive, and not always in line with provincial directives. For example, the Eden model calls for smaller units with between nine and 12 residents, while Ontario's design guidelines call for 32-bed units.

Lori Norris-Dudley, president and CEO of Osgoode Care Centre, says the home has been working for years to foster a more home-like environment for its residents. (Matthew Kupfer/CBC)
'That's where I would want to be'
Osgoode president Lori Norris-Dudley says it's worth it.
A recent trip to the Sherbrooke Care Centre in Saskatoon only strengthened her resolve to make the change.
"This is what we need to do because if I want to choose long-term care, that's where I would want to be," Norris-Dudley said in October after her visit, which she compared favourably to an Italian vacation.
"It's changing the focus from a medical model of care to a social model of care," she said.
Sheehan's daughter Katie Cote said in a previous for-profit facility, her father, who has mobility and cognitive challenges including dementia, was often referred to by his room number or legal name, John. But staff at Osgoode have really come to know him, she said.
For Sheehan, that meant small acts to help soothe his homesickness for the Maritimes, like a New Brunswick calendar, or printing out the sports schedule so he could keep up with his favourite teams.
"I feel so comforted that he's safe, he's loved, and he's heard and seen everyday," Cote said.

Katie Cote and her father Barry Sheehan in the lobby of the Osgoode Care Centre. (Matthew Kupfer/CBC)
Building a village
Osgoode has taken steps in its recreational programming and staff assignments to adopt the Eden philosophy. The building itself involves improvised touches to give it a more homey feel.
Currently, the majority of its residents live in a wing with an institutional footprint built in 1986, with a large communal dining and recreation area.
A more recent addition from the early 2000s has signage indicating "neighbourhoods" on different wings, smaller rec rooms and a gardening room. Those features help can create a sense of community among smaller groups of residents.
Osgoode's administration wants to lean into that village-type setting with another addition.
Norris-Dudley said she also plans to train personal support workers to provide a wider range of resident services rather than focusing on a narrow checklist. That could include cooking, cleaning and administering medication, she said.
She said pandemic infection prevention protocols provided a preview as staff had to be assigned to particular units, shaking up the traditional way of doing things.
"It showed how Eden would be. The staff became multipurpose. They started doing things that weren't as task-oriented, so they would be finding joy for residents because it was a horrible situation to be in," Norris-Dudley said.
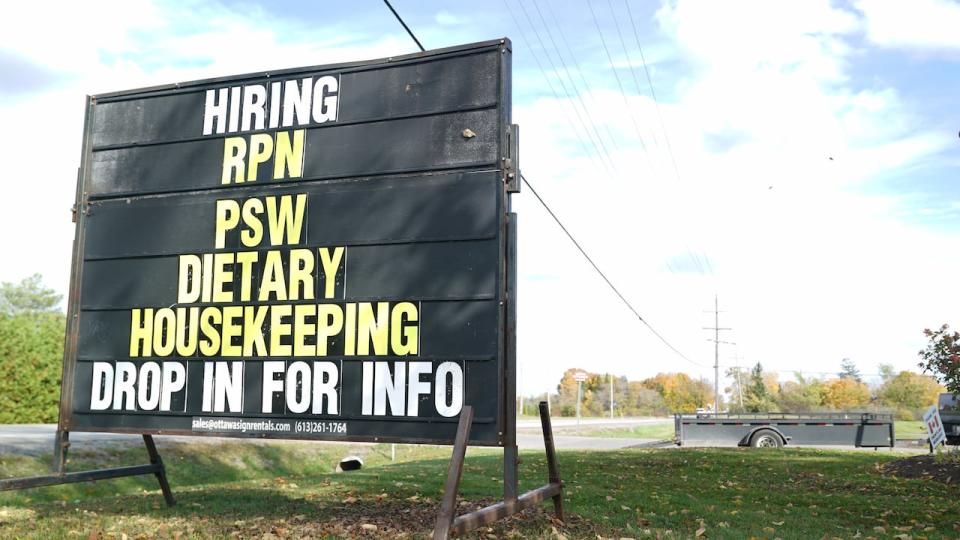
A sign outside the Osgoode Care Centre invites people to learn more about jobs at there. (Matthew Kupfer/CBC)
Norris-Dudley said she checked in regularly during the pandemic to ensure residents weren't feeling too isolated, but she also credits the tighter restrictions and the facility's rural setting for helping avoid an outbreak there until 2021.
Osgoode plans to fundraise for an expansion that would bring the Eden village to Osgoode residents because the province doesn't provide dedicated funding for those kinds of projects.
"The premier has said he supports [it] and Minister Cho has supported culture change. I just don't really think they understand it and the cost that might be associated with that," she said.
"I think the government is definitely going to have to look at top-up to support not-for-profits."
'Using available funding'
Osgoode is already in the midst of a $1.5-million fundraising campaign to upgrade its septic system — a capital project it says isn't captured in the provincial funding model.
Funding is based on the number of residents requiring a certain level of care and can be assigned to certain "envelopes" ... "to guarantee a minimum allocation of funds towards direct resident care and other baskets of essential goods and services," the ministry said.

The Osgoode Care Centre in rural south Ottawa is a non-profit, independent long-term care home. (Matthew Kupfer/CBC)
In a statement, the Ministry of Long-Term Care said all homes have the flexibility to implement the model they choose "using available funding." The ministry said it does not endorse or provide funding for any specific models of care.
Residents are required to contribute a co-payment toward meals and accommodation services, while the ministry funds nursing and personal care, the statement said.
Some jurisdictions forge ahead
Carleton University professor Susan Braedley has been studying long-term care around the world for a decade. She said homes like Osgoode have been trying to change within a highly regulated sector for decades.
"This does cost money. There are constraints in terms of standards and regulation for long-term care," she said.
Rigid meal times, for example, may help staff move from one task to another, but could lead to a resident refusing or missing a meal because they're tired or have slept in.
Similarly, while a 32-bed unit may help staff move from one task to another, it creates a less home-like environment that can be crowded and alienating for someone with cognitive issues, she said.

Susan Braedley, a Carleton University professor, has studied care models in long-term care homes in Canada and around the world over the past decade. (Matthew Kupfer/CBC)
"They reinforce sometimes some of the standards around medical care and neglect social care."
Braedley said funding for capital projects in Ontario often require administratively cumbersome application processes.
"Other provinces like Nova Scotia have gone full-tilt into changing their design standards and to support culture change," she said. "It's a shame that Ontario hasn't looked at that."
Braedley was co-author of a 2019 report for the City of Toronto that has spurred experimentation — and funding — for different care models within the municipal system.
She said there's no specific model that should be applied everywhere. Rather, individual homes should be able to pick and choose what best fits their community's linguistic, cultural, medical complexity and geographic needs.
Cote said based on what she's seen of her father's experience, she would like the Ontario government to offer more strategic support so both for-profit and non-profit long-term care homes can adopt person-focused models of care.
"It's not just making sure their medications are given to them when they need to be. It's much more than that so they can spend their senior years in a happy place and feel fulfilment from that," Cote said.

