Riverside County receives 1,000 post-exposure vaccines for monkeypox
Riverside County Public Health has received slightly more than 1,000 post-exposure vaccines for monkeypox, which would help protect 500-plus people most at risk of infection, said county spokesperson Jose Arballo Jr.
The Jynneos vaccine, approved in 2019 by the Food and Drug Administration for the prevention of smallpox and monkeypox in people ages 18 and older, requires two doses, four weeks apart. The Centers for Disease Control and Prevention is also investigating a measure to allow the vaccine to be used in children.
The county is expecting more doses to come in to help in the fight against the virus that has spread to at least 65 countries in the current outbreak, but there is no estimate as to when they might arrive.
"We continue to focus efforts on post-exposure vaccine for those who have had close contact with someone with a confirmed case, been in areas where monkeypox is spreading, or been informed by another health jurisdiction they may have been exposed," Arballo said in an email Tuesday.
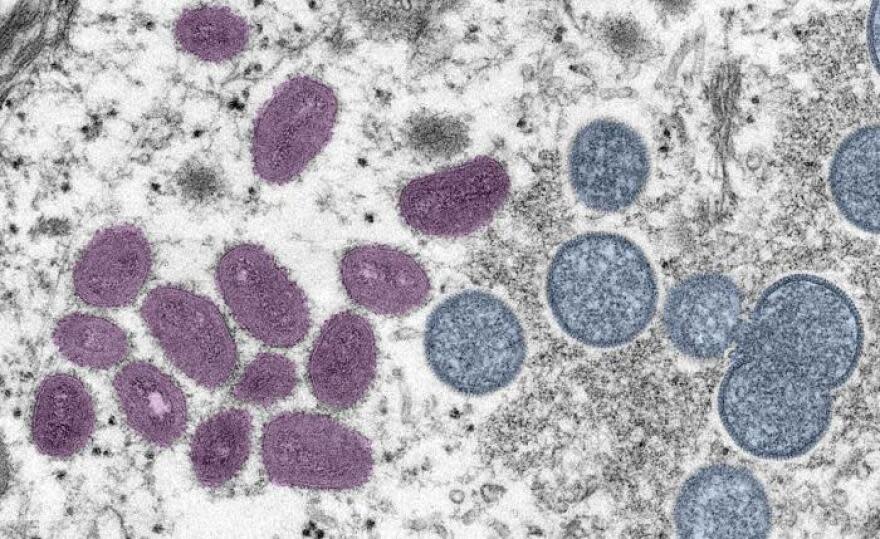
Monkeypox is a rare disease caused by the monkeypox virus. The first human case was reported in 1970 in the Democratic Republic of Congo, according to the CDC. The virus is usually found in Central and West Africa and does not occur naturally in the U.S., but recent national cases have been discovered due to international travel or animals imported from areas where the disease is more common.
Monkeypox: What Californians need to know about the virus outbreak
Read more: Riverside County outlines monkeypox vaccine distribution plan
Monkeypox is closely related to smallpox, a serious infectious disease caused by the variola virus, but is considered less deadly. According to the CDC, monkeypox is fatal in as many as 11% of people who become infected.
Barbara Cole, the director of disease control for Riverside County, previously outlined the county's vaccine distribution plan for those who have been confirmed as potentially being exposed to monkeypox. They would have a number of options to choose from to receive their shots:
If they want to get vaccinated at their health care provider, Riverside County Public Health will be able to get the vaccine to that provider within one day. If needed, the department will provide information on the vaccine and how to administer it.
People would be referred to a Riverside University Health System community health center for vaccination.
A "response team" would go out and administer vaccines.
In addition to possibly preventing monkeypox, the vaccine may also lessen symptoms in people who have been exposed.
In Riverside County, the CDC confirmed one case of monkeypox from an eastern county resident, and an additional two probable cases were reported on Friday.
People usually become infected through close contact with skin lesions or bodily fluids of infected animals or humans (alive or dead), including droplets, and can also be spread through sexual contact.
Symptoms can occur five to 21 days after exposure, and include fever, headache, muscle aches, swollen lymph nodes, rash and lesions often in the genital and perianal region. Illness typically lasts for two to four weeks.
Anyone who believes they have been exposed to monkeypox should contact their healthcare provider.
California trends, vaccine allocation
California health officials in a webinar held Tuesday discussed the latest monkeypox outbreak and the state's response in securing and distributing vaccines.
In California, there have been at least 186 confirmed or probable cases reported as of Tuesday, according to the California Department of Public Health. However, wastewater surveillance has revealed multiple positive samples from San Francisco sites and intermittent detections in Santa Clara County, Davis and Sacramento sites.
"This really implies that there's a lot more disease there than we actually realize," said state Epidemiologist Dr. Erica Pan.
Risk factors among California cases have included international travel (including noted sexual contact), close/intimate contact with a known monkeypox case, and attending large events or venues with noted skin-to-skin contact and/or multiple sexual partners. Cases have been among men and transgender men, Pan said, but emphasized that "this disease can impact anybody."
Hospitalizations continue to be rare in the United States and across the globe, Pan added.
There has been a "scarce supply" of vaccines nationally, the state epidemiologist said, but California has received around 19,500 Jynneos vaccine doses between May 27 and July 10 (56,000 vaccines available nationally). CDPH received 12,156 doses, while Los Angeles, which Pan said receives and distributes their own allocations, received 7,406 vials.
Pan said the state allocates vaccines to local health departments based on a formula that weighs the number of reported monkeypox cases and number of early syphilis cases among males.
On Monday, California ordered another 25,000 doses — 14,774 for the state health department and 9,812 for Los Angeles — among the nation's 240,000 vaccines available. For the third round of vaccine distribution, expected in September, there should be around 800,000 to one million doses available nationally. Pan said "we don't know yet what the California allocation will be." The federal government is also expected to order another 3 million doses toward the winter and early 2023.
"This is difficult and we really have to focus and prioritize how we're using this vaccine," Pan added.
The Jynneos vaccine is being prioritized for the following groups:
Post-Exposure Prophylaxis (PEP) for known close contacts of monkeypox cases
Expanded Post-Exposure Prophylaxis (PEP ++) for attendees of events/venues where known monkeypox exposure has occurred
Pre-Exposure Prophylaxis (PrEP) for individuals at occupational risk of monkeypox, such laboratory workers who perform monkeypox testing, clinicians who treat monkeypox patients and public health response personnel

One treatment available for monkeypox is an antiviral called Tecovirimat, or Tpoxx. The medication, approved by the FDA for smallpox but not monkeypox, is available in oral form (three pills taken twice a day for two weeks) or an IV.
The vast majority of people will not need the treatment, said Dr. Peter Chin-Hong, professor of medicine at the University of California in San Francisco. It will be recommended to those who have a "bad disease" — those who have been hospitalized, or who experience severe symptoms, such as confluent rectal lesions (that cause bleeding), oral ulcers (that make it difficult to eat) or lesions around the eyes — or are a "bad host" — people who are severely immunocompromised, younger than 8 years old, pregnant or breastfeeding, have inflammatory bowel disease or severe/active dermatologic disease.
Looking ahead, Chin-Hong sees four possible scenarios with the current monkeypox outbreak:
Self-limited outbreak: The virus will go away and it will be sporadic due to travel-related cases. It remains endemic in western and Central Africa.
Affects entire population: Those most at risk will be those under the age of 50 who don't have any immunity from a smallpox vaccine (stopped being distributed in 1972).
Becomes endemic: Virus gets into an animal reservoir in the United States, such as rodents or prairie dogs.
Recurrent large epidemics: It can cross from animals to humans and cause outbreaks.
"I'm hoping and crossing my fingers that it doesn't become endemic," Chin-Hong said.
USA Today contributed to this report.
Ema Sasic covers entertainment and health in the Coachella Valley. Reach her at ema.sasic@desertsun.com or on Twitter @ema_sasic.
This article originally appeared on Palm Springs Desert Sun: Riverside County receives post-exposure monkeypox vaccines

