In a Rust Belt city split by inequality, people are battling for health care justice. The fight for change is a fight for their lives.
SYRACUSE, N.Y. – Sequoia Kemp stood at the crossroads of health inequality, her mind on a painful past.
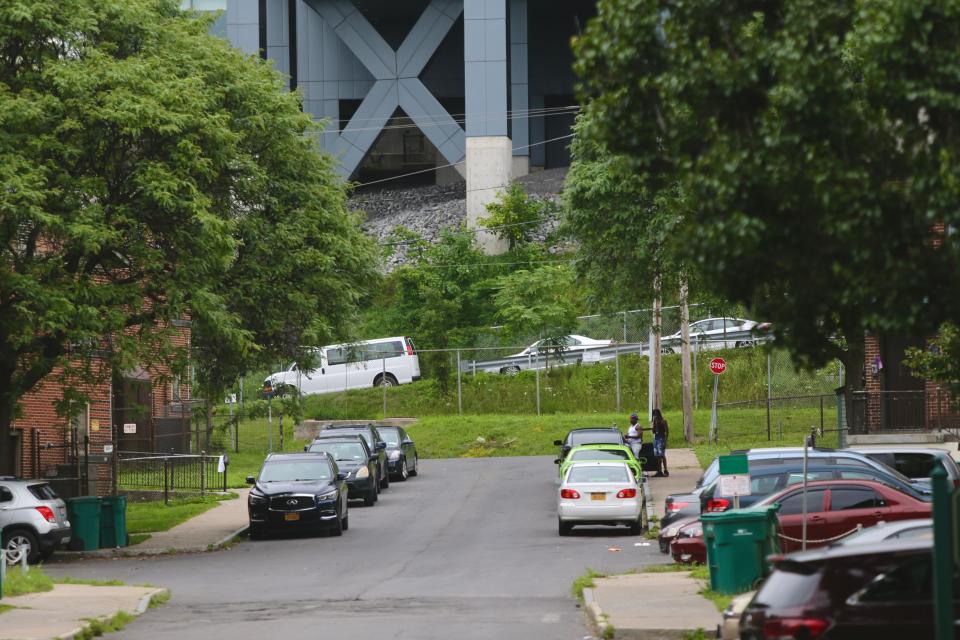
Beside her: the second-oldest public housing project in the U.S. Just above: one of New York state’s most prestigious teaching hospitals.
She took in the glimmering glass and sterile white facades of SUNY Upstate Medical University that tower over the blood-red bricks of the tenement buildings, home to mostly poor and Black people here in this Rust Belt city of not quite 150,000.
The two worlds – a shining beacon of American medicine’s bright future and stark reminder of the nation’s racially unjust present – are literally separated by an elevated highway that carved through the city’s heart decades ago.
Today, the Interstate 81 viaduct is a mass of rusting steel, chipping green paint and crumbling concrete. It is a relic of the 1950s-era urban planning that displaced and economically ravaged generations of Black and brown Americans in favor of white flight to the suburbs.
DOCUMENTARY
And it is an impossible-to-ignore symbol, many in Syracuse say, of the divisions and inequalities that put the health and lives of people of color in dire jeopardy.
On this late spring afternoon, traffic buzzed as a Black girl skipped nearby along the project's sidewalk with a cloth doll, playing amid the acrid smell of exhaust and swirling dust from construction work. A rush of memories had gripped Kemp, a 26-year-old Black woman, of a surgery she had as a teenager to remove ovarian cysts.
She remembered the month of searing abdominal pain as doctors delayed the procedure. She remembered her mother's pleas to expedite the surgery to ease her daughter's agony.

But mostly, Kemp struggled with the thought that racism marred the surgery. The unanswered questions have plagued her for years:
Would doctors have listened to a white woman and acted sooner?
Is a Black mother powerless to protect her child from medical harm?
Will I ever be able to have children of my own?
“There’s just so many stories like mine and so much trauma, and so much healing our community has to do,” Kemp said. “And I’m going to do whatever I can to be part of that.”
Those stories – of Black women emotionally and physically scarred during childbirth – inspired her to become a doula to prevent it from happening to others. She has seen countless times how the health care system treats people of color differently. She carries with her the striking truth that Black women are three times as likely to die in childbirth than white women.
On this day, she wears a T-shirt that reads: Birth Work is My Resistance.
Kemp is not alone in her fight on the front lines of health justice, in this city beset by festering wounds of racial segregation and stunning inequality. There are agents of change on both sides of the divide, here in the heart of the city and high on the hill inside the halls of medical healing.
The struggle to find basic care: Sickle cell children are living longer than ever, but as adults they face challenges to get basic care
But the stakes are crystal clear. They are written on the faces of the expectant mothers Kemp helps, etched in the well-being of her own body, evident in the everyday discrimination that targets the people she loves.
It's a fight for the lives of women. For friends and her family. For herself.
“The first thing most of my clients say,” Kemp said, “is ‘I don’t want to die.’”
An American health crisis
In Syracuse and across the country, a new generation of activists and medical professionals — many of them forged by their own health-related trauma — are leading the charge to end the systemic inequalities that ensure Black, Latino and Native American lives are less healthy than white lives.
Here, they are the people pushing plans to tear down Syracuse’s highway system and seeking reparation. The roads' racially biased placement killed the American dream of their ancestors, who fled the Jim Crow-era South only to find a Northern city being segregated by its own brand of discrimination.
They are also the medical students who are exposing untold and ongoing harm caused by attempts to justify American slavery with theories that Africans’ “race” was inferior to whites.
And they are the scholars unraveling the legacy of slave-owning doctors claiming Africans’ comparatively weak bodies benefited from grueling slave labor.
They are behind a growing movement to reject the racial inferiority theories, which remain in the bedrock of modern medicine despite being disproven and have fueled the mistreatment of generations of Black Americans.
‘I don’t think you are ready’: Boys of color fell further behind at school amid COVID-19
This movement is part of a much broader struggle to improve the quality of life for those excluded from the American social contract. When it comes to keeping people of color healthy — and healing them when they are not — endless factors play a role, from the environment to access to care centers, from insurance plans to steady incomes, from nutritious meals to medical mistrust built on centuries of trauma.
The health-justice movement aims to end racist housing policies that place more Black children near toxic fumes and exhaust, contributing to them having asthma-related death rates eight times higher than whites.
It requires eliminating food deserts and medical distrust linked to Blacks being twice as likely to die of diabetes than whites. And removing unjust economic policies and practices linked to Black people being 30% more likely to die from heart disease than whites.
The endeavor also targets the medical deserts and low-wage jobs linked to Blacks, Latinos and Native Americans that were put at twice the risk of dying from COVID-19 than whites.

“Racism is not just the discrimination against one group based on the color of their skin,” Centers for Disease Control and Prevention Director Dr. Rochelle Walensky said in April, declaring racism a national public health threat.
Rather, it is “the structural barriers that impact racial and ethnic groups differently to influence where a person lives, where they work, where their children play, and where they worship and gather in community,” she added.
Undergirding it all is the tectonic push for truth in medicine, as revelations surrounding complex clinical algorithms used to make race corrections to treatments suggested millions of Americans were mistreated for decades.
COVID and race: CDC declares racism a 'serious public health threat' as COVID-19 puts a spotlight on disparities
USA TODAY Network journalists assembled a complex assessment of these intertwined issues by interviewing Americans from across the country, revealing the lives devastated by health inequality, as well as their fight for better treatment. They also analyzed health data and federal records detailing the misuse of race in medicine to shed light on the massive systemic reforms needed to end disparity in health and health care.
The outcome of the heated debate among health care leaders over race-based corrections in particular could save lives and prove crucial to building trust with people of color.
“More and more medical groups are realizing that race corrections are both on the wrong side of history and on the wrong side of evidence-based medicine,” said Dr. David Jones, a Harvard University professor. “I hope people of color would look at this and say doctors are really trying to look at this and figure out what is going on.”
Tales of racism, health and inequality in an American city
In Syracuse, which has some of the poorest neighborhoods in the country, tales of unmet health needs, unsafe housing conditions and unequal access to health care unfold daily.
Deka Dancil grew up Black in extreme poverty, eating cheese slices and drinking hot sauce for days at a time when her family’s food stamps ran out. She spent her teen years sleeping on couches at homes of friends and relatives and worked her way through high school as a janitor at Upstate Medical University.

“I would have never believed, or had the audacity to think, that if there was something I needed that I would be important enough for the top specialists at Upstate to care for me,” said Dancil, 28, and now president of the Urban Jobs Task Force.
As a Medicaid patient, she added, her care was always funneled to the federally qualified health center, which lacked the expertise and resources available at Upstate.
Lily Sanders, a 67-year-old Black mother of three, grandmother of 11, and great-grandmother of four, has taken pride in working low-wage jobs at Syracuse-area nursing homes. But she's remained unable to afford health insurance premiums and deductibles most her life.
Instead, she has prayed to stay healthy and out of the emergency room, while living among the boarded-up Victorian homes and gang violence that have blighted the city for decades.
“It’s very scary. I’ve been blessed with good health, and every day you’re hoping that you don’t need anything,” Sanders said.
She described herself as one of the millions of working-poor Americans, earning above the Medicaid threshold but unable to afford health insurance costs. She has often turned to the Poverello Health Clinic, a free health center in Syracuse, for minor care while forgoing most dental treatment.
“It affects people of color because they came from a place of zero — from slavery,” she said. “You try to get something, but the system doesn’t allow you to get anything…You just can’t get a toehold and you just never get up.”
The preventable suffering is clear for Rachel Johnson, a 25-year-old community advocate, gently urging a Black man with diabetes to visit doctors and eat healthy. His diet consists mostly of offerings at the corner store advertising beer and cigarettes, rather than fruits and vegetables available at grocery stores in less poverty-stricken neighborhoods.
“There is long-standing intergenerational trauma that is baked into people of color,” said Johnson, director of health services at Syracuse Community Connections. “Some of the bigger issues of mistrust in health care are connected to some of those historical factors.
Disparities in the US: COVID deaths third after heart disease and cancer in US last year; people of color hit hardest, CDC reports confirm
“This is national. It’s not just one local entity, or just one city … it is across the board,” she added.

In Syracuse, the health inequity crisis has also manifested in the stunted lives of at least 675 children poisoned by lead paint in 2017 alone, many of them living in the city’s aging housing stock still filled with lead-based paints that were banned in 1978.
Then there is simply the fact kids in Syracuse with asthma are more than twice as likely to end up in the emergency room than peers in surrounding suburbs, including cases linked to traffic-related air pollution from living in the highway system’s shadow.
But life on this side of I-81 has helped prompt a push for change on the other side, where three Black women studying at Upstate Medical to become doctors have turned their personal clashes with discrimination into a collective attempt to achieve health justice in their town.
How racism sparked a path to med school
Eight-year-old Isabelle Thenor-Louis saw racism unfold one evening through the window of her own home.
Her father had pulled his car into their driveway in the wealthy, and mostly white, Long Island neighborhood where they lived. A police car stopped on the street with its engine idling as the Black man, a doctor, slowly walked towards that house that officers wrongly assumed he couldn’t afford.
Under the glare of racial profiling, Isabelle's dad entered the front door. He embraced his family, and a few tense moments crept past before the police sped away.

It left the first of many scars in a rising American family’s struggle against racism.
Today, a 26-year-old Thenor-Louis recalled such episodes — including a patient mistaking her father for a janitor — as sparks that ignited her path to medical school.
“It’s one of those things that snowballed as you’re growing up and you start to realize, ‘OK, I’m not really seen as someone of value,’” she said. “As a Black woman, I saw it was really important to be part of the solution.”
Her realization expanded recently after she complained of health and skin issues common among Black women during medical visits, only to be dismissed by white doctors. When she visits doctors now, she wears a sweatshirt emblazoned with the insignia of her alma mater, Brown University, to combat racial bias, implicit or explicit.
“It’s unfortunate that I feel like I have to put on all these physical qualifiers to show I have value and should be treated equally,” Thenor-Louis said. “It’s almost like preparing to go to battle.”
Today, she is working towards becoming a hybrid physician-journalist in the mold of CNN’s Sanjay Gupta, hoping to improve the health of people of color while sharing their stories to the world to effect change.
Entering the medical field: Medical school applications surge as COVID-19 inspires Black and Latino students to become doctors
Yet her trials at getting this far underscored the challenges behind the shortage of doctors of color, which span a range of economic and social barriers to medical school.
While the number of medical school spots has increased by 27% since 1981 overall, just 13.7% of the medical student population is from Black, Latino, American Indian or Alaska Native communities. That’s despite these underrepresented groups composing 35% of the U.S. population. Meanwhile, just 3% of doctors nationally are Black women.
And while research shows people of color are healthier when treated by doctors of color, advocates have long stumbled in closing the diversity gap. An effort stalled by the burden of more than $200,000 in medical school debt on average and racially segregated educational opportunity.
The pandemic’s uneven toll in communities of color, however, may turn the tide. The suffering contributed to an 18% surge in medical school applications for the fall, according to the Association of American Medical Colleges.
Further, many of the aspiring doctors are people of color inspired to remedy the health inequalities laid bare by the coronavirus, as scholarship programs, educational outreach and free tuition initiatives seek to remove barriers to medical school.
The importance of closing the divide between the ranks of doctors of color and an increasingly diverse nation of patients struck close to home for Samantha Williams, another Black medical student at Upstate.
Born and raised in Syracuse, Williams moved to the suburbs as a teen with her mother, a widow, and two siblings. Her only ticket to studying medicine: a scholarship promoting medical school diversity.
She's faced many microaggressions as a Black woman in a predominantly white environment, she said.
Recently a campus safety alert had Upstate Medical students’ smartphones buzzing, warning of a stabbing in the public housing projects near campus. Williams overheard a classmate sarcastically declare, “Classic Syracuse.”
“It’s hard sometimes to hear that about my hometown,” she said.
During another class, Williams found herself with other students of color raising their hands when a professor asked if they’ve known a victim of gun violence, leaving her shocked that other white students hadn't been affected.
The incidents were among many reasons Williams worked with Thenor-Louis and their classmate, Angelina Ellis, the daughter of Jamaican immigrants, to organize the Health Justice at Upstate conference in January.
The virtual event drew hundreds of attendees and focused on connecting medical students, doctors and Syracuse community leaders to pursue local projects to reduce health inequity.
“I have the greatest hopes that people understand the communities they’re treating,” Williams said.
The search for racial truth in medicine
In Syracuse, young students and community outreach workers are leading the charge for systemic change. And in some ways, the history of doctors misusing race in American medicine began unraveling in a Harvard lecture hall.
There, medical students began questioning methods used to adjust treatments based on a patient’s race. Several of the students turned to David Jones, a Harvard professor specializing in race, technology and the culture of medicine, to find answers.
The resulting medical paper, Hidden in Plain Sight, published in August in New England Journal of Medicine, would raise questions about flaws in race-based medicine that some experts say were harming people of color.

“There’s such a pervasive assumption in U.S. society and U.S. medicine that Black and non-Black people are different; I don’t think anyone stopped to look twice,” Jones said.
“It’s often the people who are new to a profession who are going to be alert to something that members of the status quo can’t see,” he added, praising medical students for opening the racial justice floodgates in health care.
The group’s probe of medical race corrections detailed how complex health-related math equations and risk calculators contributed to unequal care for whites and people of color.
Due to the algorithms, many Black men and women may have received delayed or lesser care for kidney, heart and lung diseases, the research suggests, and women of color potentially received less-aggressive cancer screening.
Some Black and Hispanic women may have been improperly advised against pursuing vaginal birth after a cesarean delivery, exposing them to a serious operation while robbing them of a personal choice more widely offered to white women.
And race-adjusted treatments may have perpetuated health disparities, rather than resolving them, by directing more medical resources to whites than people of color, according to the research.
In other words, using faulty and biased health data potentially engrained the negative effects of racism and discrimination into the medical system.

The real-world stakes of the research have played out for Kemp, the Syracuse doula, who recounted getting a panicked call one day from client on the verge of childbirth. A doctor was advising the Black woman against pursuing vaginal birth due to a prior C-section delivery.
Kemp raced to the hospital, explained the woman’s desire to pursue a vaginal birth and effectively overturned the doctor’s advice. She called it one of her numerous confrontations over treatment decisions.
“Internally there is a lot of anger, especially because I feel like a lot of providers are not giving the full benefit and full risk to patients of color,” she said. “They tell my clients what they’re going to do to their body instead of asking them.”
“It’s very enraging because providers want people to trust them, but how can you expect them to trust you when you’re not asking permission to touch them?” Kemp added. “The model of care is scaring people because of that real-life fear of racism, and Black women going into routine childbirth and dying.”
Ending centuries of racist medicine
The race-based medicine debate, however, may have gone unnoticed by most people outside health care circles if the murder of George Floyd, a Black man, at the hands of a Minnesota police officer hadn’t triggered a social justice movement last summer.
“The discourse now in health care is totally different than it was before Mr. Floyd’s death,” Jones said.
Top medical associations and hospitals across the country have since faced a moment of reckoning around race-based medicine, fueled in part by a Congressional inquiry of the issue.
Lawmakers have pushed for systemic reforms related to the article’s findings, which also gained momentum following a lawsuit alleging racially-biased dementia tests in the NFL’s concussion litigation resulted in uneven payouts to Black and white retired players.
Lawyers: NFL concussion awards discriminate against Blacks
As a result, some hospitals have abandoned the use of certain race-based clinical methods over the past year. Other health institutions and medical groups are backing efforts to better account for and counteract racism’s ravages on health throughout American history.
Indeed, race corrections in American medicine traced to Thomas Jefferson’s Notes on the State of Virginia in 1832, which noted deficiencies of the “pulmonary apparatus” of Blacks, said Stephen DiCarlo, a professor at Michigan State University.
“Plantation physicians used Jefferson’s statement to support slavery, believing that forced labor was a way to ‘vitalize the blood’ of deficient black slaves,” DiCarlo wrote in a 2018 article in Advances in Physiology Education.
Today, doctors still use a medical device called a spirometer to measure lung function and make race corrections, despite its historic connections to Samuel Cartwright, a Southern doctor and slave owner.

Much of the research supporting the lung-related race corrections, however, fails to properly account for social and economic factors harming Black patients’ lungs, underscoring the need to better understand racism’s toll on health.
Meanwhile, debunked theories asserting African-Americans may have a gene predisposing them to higher blood pressure than whites continue to circulate widely in some medical circles and the public, DiCarlo said.
The disparity was initially attributed to Africans living in a dry climate being able to retain more salt. Its defenders then tweaked the theory to incorporate slaves who survived the brutal passage over the Atlantic Ocean, asserting the gene shortens the lives of their ancestors.
“It’s not true, but it’s something that we simply keep repeating and repeating and now it is part of society,” DiCarlo said.
The truth, DiCarlo and other experts say, is Blacks disproportionately suffer from higher blood pressure than whites due to a range of societal factors, including the regular release of fight-or-flight hormones triggered by everyday racism.
Meanwhile, some medical groups have recently asserted clinical algorithms will soon be replaced by unbiased methods that better represent the fact that race is a social, not a biological, construct.
Some ongoing research, such as a project at Mount Sinai Health System in New York, also aims to improve the understanding of both environmental and genetic factors underlying diseases and, ultimately, devise better treatment plans.
Yet some doctors and medical groups, including the National Kidney Foundation of America, have asserted removing clinical algorithms without replacing them with better methods may cause more harm than good, citing how health disparity predated algorithms.
“If we have institutions that are doing this in different ways, we have a problem,” said Dr. Neil Powe, chief of medicine at Zuckerberg San Francisco General Hospital and member of the kidney foundation’s task force studying the issue.
“A patient would go to one system and be told they have kidney disease and go to another and be told they don’t; that is chaos,” he said. “What we all need to do is to find a path forward together so that we are all in-sync for the benefit of patients."
Building health equity
Despite its history of discrimination and segregation, the city of Syracuse, where nearly half of children still live in poverty, offers a case study in the new strategies being deployed to curb social and health inequality.
A $1.9 billion project is planned to replace the elevated I-81 viaduct with a community grid conducive to local businesses and neighborhood growth.
Local, state and federal officials have touted it as a testament to the national push underway to undo the follies of racist urban planning over the past century.
Further, a plan is progressing to redevelop the Pioneer Homes public housing project near Upstate Medical. It aims to create mixed-income apartments to end the cycle of poverty and violence that have defined the neighborhood, which was built around 1940.

The moment stands in stark contrast to the leadership that built the highway system in the mid-1960s to destroy Syracuse’s old 15th Ward, where 90% of the city’s Black residents lived due to housing discrimination, according to Onondaga Historical Association archives.
“Syracuse is not unique in this,” said Gregg Tripoli, executive director of the group. “Many other American cities are now beginning to grapple with issues that we have needed to address for a long time.”
In fact, hundreds of road and bridge construction projects tied to racial justice initiatives could unfold across the country, as President Joe Biden’s administration supports the effort in its $1.2 trillion plan to rebuild the nation’s aging infrastructure.
But advocates have raised concerns the new urban planning projects have yet to provide enough details to ensure history’s mistakes aren’t repeated. Their concerns include minorities being underrepresented in the construction jobs, as well as gentrification displacing the people of color currently living near the roadways.
“We stress how many Black people were affected by this highway just because they lived there, and it’s crazy because they’re being targeted to have that happen to them again,” said Dancil, who is also manager of bias response and education at Syracuse University.
When the I-81 viaduct was built, Dancil’s great-grandmother, grandmother and other relatives were among the thousands of Black people living in the 15th ward due to redlining, the housing segregation practice linked to the federal Housing Act of 1949, she said.
Today, the city’s concentrated pockets of extreme poverty nearly mirrored the redlined neighborhoods established more than 70 years ago, she added.
Yet despite the massive scope and generational implications of the highway replacement, improving the health of those living in Syracuse has also involved seemingly small victories.

For Luvenia Cowart, a Syracuse University professor specializing in health equality, a group of pastors declaring their African-American church functions “fry-free zones” offered some of the first glimmers of hope for ending health disparity in Syracuse.
Instead of potato salads, fried chicken, Kool-Aid and soda, the church dinners and picnics began offering tossed green salads, baked chicken, milk, water and tea, as part of a community-wide push to curb obesity.
“It may appear to be a small thing, but it’s huge when you can over time see the difference in how meals are prepared and the food choices among people,” Cowart said.
The change stemmed from the Genesis Health Project that Cowart founded in 2004. It started with six inner-city Black churches and now encompasses 14 congregations, which participate in a variety of health literacy programs targeting issues in the Black community.
From encouraging men and women to seek cancer screening to facilitating care for dementia and diabetes, the project has seen incremental progress in improving health outcomes. And the key to success has been partnering with the churches that remain the cornerstone of the Black community.
“The bottom line is establishing relationships and establishing that level of trust,” Cowart said. “Because we have worked in this community for a very long time, and to a large extent are part of the community, we are trusted.”
As Syracuse and the nation seem poised to tackle some of the iconic barriers to health equity, including the highway systems, Cowart cautioned against losing momentum in tackling other social, economic and environmental factors harming people of color.
“This did not happen overnight, and the solution is not a quick solution,” she said. “This is a step-by-step process that is going to take time, but we need to be focused and we need to continue the journey because there are people that are suffering and dying.”
David Robinson is the state health care reporter for the USA TODAY Network New York. He can be reached at drobinson@gannett.com and followed on Twitter: @DrobinsonLoHud
Read the previous installments of Justice In My Town
Heart of the movement: How these 12 young activists are seeding change in their towns
Three communities show how government actions perpetuate racism in our town
More in this series
In a Rust Belt city split by inequality, people are battling for healthcare justice. The fight for change is a fight for their lives.
'Who is going to help me?': How a Florida team brings healthcare to the community
How gaps in health insurance coverage haunt vulnerable patients
Food deserts in the Port City: Limited access endangers health, and this town is fed up
'Meeting people where they are': How understanding Austin's people is key to vaccine push
'You're the only Black person that you see': Why support is vital for medical students, doctors of color
The team behind Justice in My Town - Health care crisis
DOCUMENTARY VIDEOGRAPHY AND PHOTOGRAPHY: Robert Bell (Rochester, N.Y.), Kenneth Blevins (Wilmington, N.C.), Richard Burkhart (Georgia), Shawn Dowd (Rochester, N.Y.), Alex Driehaus (Naples, Fla.), Andrea Melendez (Naples, Fla.), Ana Ramirez (Austin, Texas), Tania Savayan (Westchester, N.Y.), Alyssa Vidales (Austin, Texas)
REPORTING: Tom Corwin (Augusta, Ga.), Brian Gordon (North Carolina), Hannah Ly (Rochester, N.Y.), Luz Moreno-Lozano (Austin, Texas), David Robinson (New York), Janine Zeitlin (Naples, Fla.)
DATA VISUALIZATION: Janie Haseman (USA Today)
EDITORS: Michael Kilian, Kristen Cox Roby, Carrie Yale
DIGITAL PRODUCTION AND DEVELOPMENT: Spencer Holladay, Diane Pantaleo
SOCIAL MEDIA, ENGAGEMENT AND PROMOTION: Mason Callejas, Sarah Duenas, Kara Edgerson, Ana Hurler, Sarah Robinson
This article originally appeared on New York State Team: Racism, inequities in health care has long history in Syracuse, NY

