‘I screamed in non-stop pain for 45 minutes’

- Oops!Something went wrong.Please try again later.
“The pain was so terrible I couldn’t move, turn over, or sit up. I screamed non-stop for 45 minutes,” said BBC presenter Naga Munchetty earlier this week, as she described how she suffers with adenomyosis, a debilitating womb condition.
“Constant, nagging pain. In my uterus. Around my pelvis. Sometimes it runs down my thighs. And I’ll have some level of pain for the entire show and for the rest of the day until I go to sleep.”
You might not have heard of adenomyosis – but it’s as common as its relative, endometriosis, affecting up to one in 10 women.
The condition occurs when the tissue that normally lines the uterus grows into the muscular wall of the uterus, and continues to thicken, break down and bleed, during each menstrual cycle.

An enlarged uterus and painful, heavy periods can result. Doctors aren't sure what causes adenomyosis, but it’s most common in women aged 35 to 50, and usually resolves after menopause.
The illness causes heavy and painful periods. It can also have an impact on fertility and may lead to anaemia from menstrual blood loss.
Adenomyosis forms areas of little cysts that each month tend to grow and bring about pain and bloating.
Adrian Lower is a consultant gynaecologist at the Princess Grace hospital in London. “It is a bit like having a bruise within the uterus,” he says. “This might result in pain with sex, pain with opening the bowels, pain with menstruation.”
How is adenomyosis diagnosed?
The condition is diagnosed with an ultrasound or MRI scan, which, if adenomyosis is present, will show an enlarged uterus, with one wall of the uterus thicker than the other.
The condition is often confused with fibroids, says Lower, which are non-cancerous growths that develop in the muscular wall of the uterus. Some doctors will recommend an MRI scan, he says, as it is easier to differentiate between fibroids and adenomyosis on an MRI scanner than an ultrasound scanner.
How is it treated?
In the past, treatment options were limited for women with adenomyosis. “25 years ago, adenomyosis was the most common cause of hysterectomy”, says Mr Joseph Aquilina, a consultant gynaecologist at St. Bartholomew’s and the Royal London Hospitals. Fortunately, today, there is a range of less drastic treatments on offer and most of these seek to manage the symptoms of the condition.
“In the majority of cases”, says Lower, “adenomyosis is best treated by suppressing menstruation”.
The hormone progesterone is used to prevent a woman from having her period, which means she won’t experience the severe menstrual pain or bleeding that occurs with adenomyosis.

Progesterone can be taken orally, in the form of the combined contraceptive pill or progesterone-only mini pill, transdermally, as injections, or through the uterus.
The Mirena coil, which is an intrauterine device (IUD) that secretes progesterone, is Lower’s preferred treatment. “It is the best because the progesterone binds to the receptors in the uterus and that is the first place the progesterone hits and suppresses the growth of the endometrium.”
But hormone treatments aren’t for everyone, Aquilina cautions. “Some women may not be able to tolerate progesterone and could experience side effects that include depression, breast tenderness, acne and headaches”.
He agrees, however, that the Mirena coil is a favourable option as it offers, “a very small dose of progesterone, about a hundredth of the dose,” compared to the oral contraceptive pills.
It might be an attractive solution for women who experience side effects with progesterone and is about 60-70 per cent effective in terms of reducing blood loss and pain.
The surgical option
There is also a one-off procedure called an endometrial ablation, where the lining of the womb is removed, sometimes with radiofrequency, sometimes with heated fluid. It is very quick – the process itself can take as little as 90 seconds – and some hospitals will do the procedure under local anaesthesia.
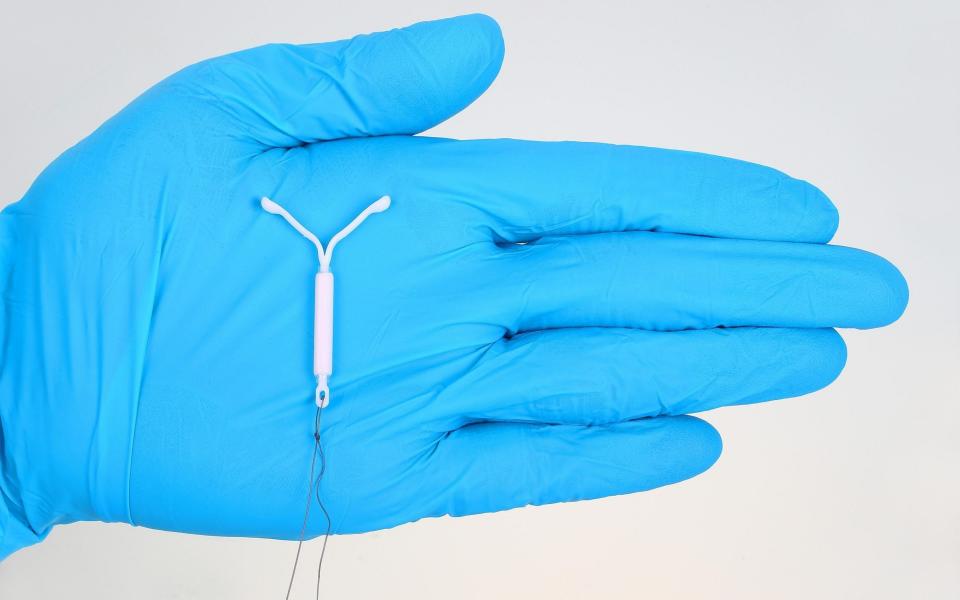
Like the Mirena coil, its efficacy is around 60-70 per cent and it is even better when it is combined with the coil, a combination treatment that is now recommended by the NHS.
The downside of endometrial ablation is that it isn’t suitable for women who might want to get pregnant as it permanently impairs fertility.
Although adenomyosis is found most often in women between the ages of 40 and 50, it can also present in women in their twenties and thirties. For women who would not wish to undergo a procedure that would impact their fertility or take medications to suppress menstruation, there are non-hormonal treatments.
These include medications to make the periods less painful, such as mefenamic acid, and tranexamic acid to reduce bleeding.
“It is very rare for adenomyosis to end in hysterectomy now,” says Aquilina. “There is a small percentage of women, and these would usually be patients who have endometriosis or fibroids as well.”
What’s the prognosis?
The outlook for patients who have had endometrial ablation combined with the Mirena coil is particularly good, with 90 per cent of women not coming back to request a hysterectomy.
Opening up about her struggles with the condition, Munchetty said that, before she was diagnosed, she experienced decades of painful, heavy periods. One of the reasons that adenomyosis often goes undiagnosed is because pain is an expected part of menstruation.
Many women don’t know what an abnormal level of pain is or when they should consult a doctor.
As adenomyosis is a chronic condition that will worsen over time, Lower encourages women to, “seek medical opinion if there is a deterioration in symptoms.”
Aquilina says that any woman whose quality of life is being impacted every month by their period should see a GP. “A red flag would be if she is having one or two days a month when she is completely incapacitated, when she cannot function.”

