Seems like COVID, flu cases are on the rise in Texas? You're right. What you need to know.
You are not imagining it. Respiratory viruses are circulating en masse across Central Texas, from severe cases of the flu to COVID-19, respiratory syncytial virus (aka RSV) and even some strep.
We talked to three doctors — who work in primary care and urgent care along with an infectious disease specialist for a hospital system — to ask what they are seeing.
What's going around? Start with COVID-19
The most common thing circulating now is COVID-19, followed by flu A and then some RSV.
"COVID-19 has never gone away," said Dr. Angela Gibson, director of urgent care services and after-hours clinics for family medicine at Austin Regional Clinic. Instead, it has spikes, typically in summer and then winter, beginning in late November into December and January.
We are in a spike currently, fueled by holiday travel and gatherings.
Yes, the flu is much worse this year
The flu is definitely worse this year than in 2021, 2022 and 2023. The good news? It's not as bad as in 2020 just before COVID-19 hit, she said. The flu A strain right now is causing about three-fourths of the cases compared with flu B. The two strains are very similar in symptoms, though flu A can be more serious in adults and flu B more serious in children.
Why is flu so bad this year? Call it the "great unmasking." Gibson said we stopped wearing masks, and we went out into crowds again. Our bodies have forgotten what the flu is after a couple of years of not experiencing it, so we don't have as much immunity without vaccination or experiencing it again.
People can have flu and COVID-19 or RSV at the same time. They can also get flu A, get better and then contract flu B.
Similar symptoms? Get tested.
All these respiratory viruses have similar symptoms, which can make them hard to distinguish, said Dr. Sue Inonog, internal medicine doctor at Harbor Health.
Anyone with coldlike symptoms of a runny nose, cough, sore throat, body ache should be tested for COVID-19 and flu.
With older people or the very young, an RSV test is often done to protect the most vulnerable from spreading it. People with a sore throat should be tested for strep.
All these respiratory illnesses can lead to a secondary infection like bronchitis or pneumonia. With flu, pneumonia can happen as early as the second day.
Symptoms? Here is a guide from doctors
Doctors have seen people who have flu look sicker and feel sicker than people with COVID-19. Flu tends to come on very quickly and to cause a high fever and body aches.
COVID-19 tends to be milder. COVID-19 patients think they have cedar fever or another allergy. They are surprised when the COVID-19 test comes back positive, Gibson said.
People with RSV often are wheezing or suffer difficulty breathing. RSV can take weeks for the cough to go away. Before we had testing for it, RSV was a common winter cold with no name. Look out for secondary infections in the ears and sinuses, and possibly pneumonia weeks later.
How do viruses spread? Yes, COVID-19 is most contagious
COVID-19 remains the most contagious because it is airborne, carried in respiratory droplets and transmitted by exhaling, coughing and sneezing. While flu is airborne, it is not as contagious as COVID-19. Other viruses spread when people share drinks, food, saliva or those viruses fall on objects or surfaces that you touch and bring to your mouth or nose.
Strep and RSV tend to happen more in children or people who come into contact with children. Sometimes with strep, one family member gets it, has a fever, then feels fine and never knew they had strep, until the next family member gets it and is much sicker with the classic bad sore throat.
How about your stomach?
It's not just the respiratory crud. Holiday weeks come with two versions of gastrointestinal illness. Some cases are viral and include stomach upset, vomiting or diarrhea. The rest are food-borne from eating out or from leftovers that sat out or have not been reheated or cooked properly.
Holidays are over. Are viruses done? Flu has not peaked!
Nope. Kids return to school, which means different germs. Flu tends to build in December and January with a spike in February before the numbers fall. With flu, "we're not at the peak yet," said Dr. Brian Metzger, medical director of infectious diseases at St. David's HealthCare.
Sometimes in a flu and RSV season, these viruses will diminish and spike again. Metzger's fear is that COVID-19, flu and RSV will spike together, which happened in October and November of 2022 — leading to no pediatric hospital beds being available in Austin.
Are the hospitals inundated with cases of COVID-19?
No. It's not like previous years, but people are hospitalized in Austin because they have COVID-19 or flu, Metzger said. They tend to be in the hospital because they also have comorbidities such as heart, lung or other organ problems. They also tend to be older.
Metzger has been treating patients who are otherwise healthy and as young as in their 20s who have COVID-19 or flu that got serious quickly. He sees a lot of post-viral infection bacterial pneumonia that occurs when the immune system is weakened by COVID-19 or flu and a secondary infection occurs.
People still die from these diseases, he said, but this is rare.

Should we mask again?
"I don't think anyone has the stomach for mandates or anything like that," Metzger said.
People should consider wearing masks in crowded spaces like airports and airplanes if they are in a high-risk category for a bad infection because of their age or immune system. If they have someone at high risk in their house, they might also consider wearing a mask in public spaces to keep that person safe.
There should be no "mask-shaming," Gibson said, because you never know if that person has immunity issues because of cancer or a transplant or other health reasons.
What to do if you are sick? A guide
The rule of thumb for most viruses: You can return to work or school if you have been fever-free for 24 hours without fever-reducing medication. The exception is COVID-19. You must isolate from everyone for the first five days, with day one being the day you had a fever, began feeling bad or the day you tested positive. After those five days, you need to wear a mask for the next five days, for a total of 10 days of isolation/mask wearing. That mask needs to be an N95 or a KN95.
How stay healthy during cold and flu season
Test for COVID-19 if you just don't feel good or think you have allergies.
Call your doctor if you think you have COVID-19 or flu. There are antivirals to lessen the symptoms. The one for flu is given within 48 hours of the start of the virus; the one for COVID is within the first five days.
Stay home if you are sick.
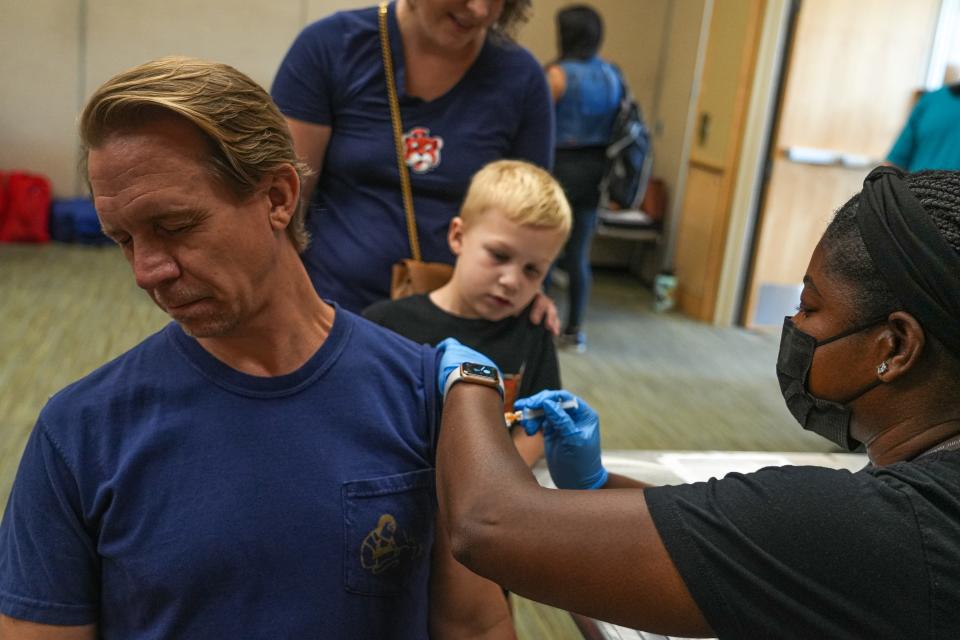
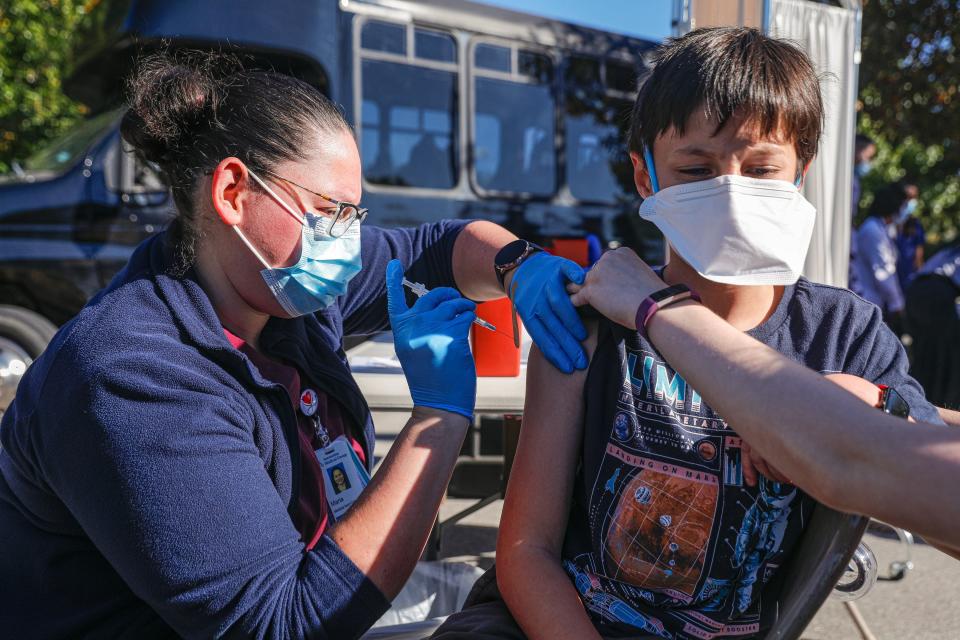
Get vaccinated. It is not too late to get the new COVID-19 booster or a flu shot or the RSV shot if you are 60 years old or older. Flu and COVID-19 vaccines only cover you for about six to 12 months before they start to wane. These viruses mutate every year, so you need to get the most current booster each season. If you do not have health insurance or cannot afford a vaccine, Austin Public Health offers vaccines for $25 for adults and $10 for children. Call 512-972-5520 for an appointment.
Wash your hands.
It never hurts to wear a mask in crowded spaces.
This article originally appeared on Austin American-Statesman: COVID, flu cases rise in Central Texas. Everything you need to know.

