‘System is broken’: NH mental health centers seek $30M to add workers, bolster treatment
- Oops!Something went wrong.Please try again later.
The state has spent millions to expand mental health treatment in the last two years. Yet those who need it are still waiting. In emergency rooms, some for days. At home for a mobile crisis team that’s an hour-plus away. For a counseling appointment. For housing after psychiatric hospitalizations.
Mental health advocates say there are consequences to a shortage of care. Patients who put off cancer or cardiac treatment during the pandemic saw their conditions worsen, and the same is true for people unable to get timely mental health treatment.

“It’s like telling a pregnant woman, ‘Cross your legs and wait,’ ” said Maggie Pritchard, president of the New Hampshire Community Behavioral Health Association and chief executive officer of the Lakes Region Mental Health Center. “You can’t really do that if somebody’s having a psychotic episode and needs help.”
The association’s 10 community mental health centers, which treated about 60,000 people last fiscal year, most insured by Medicaid, have told Gov. Chris Sununu they need an additional $26 million to $28 million a year to address those wait times. To cover the cost, they have proposed the state increase its Medicaid reimbursement rates, which fund about 70 percent of centers’ budgets, and don’t fully cover the cost of providing care.

“Except for the last biennium (when centers saw about a 3.1 percent rate increase both years), that fee schedule that drives our payment hadn’t changed in 20 years,” said Roland Lamy, the association’s executive director. “You can quickly see that inflation is inflation is inflation and we’re not immune to it.”
The budget increase, which would require a 21.5 to 23 percent increase in the reimbursement rate, would support two critical needs, Lamy said: recruitment and retention and supported housing.
More:Teens tell their truth about social media and mental health. 'I always have my phone.'
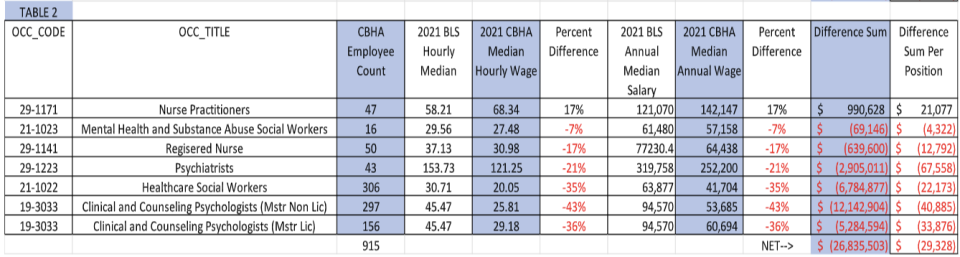
With nearly 340 clinical vacancies, the centers have requested $26 million to $28 million to increase wages, which Lamy said lag 7 to 43 percent behind national wages reported by the federal Bureau of Labor Statistics. The median annual salary for the centers’ psychiatrists is nearly $68,000 less than the national median salary. Registered nurses make about $13,000 less a year, psychologists as much as $40,000 less.
The centers have also requested an additional $1.5 million to add 60 community-based “step-down” beds for people who don’t need hospitalization but can’t yet live independently. The dire shortage of all housing options prevents New Hampshire Hospital from releasing patients who are ready for discharge but have nowhere to go. Jake Leon, spokesman for the Department of Health and Human Services, said 50 patients were awaiting discharge, each of them claiming a bed, while 44 adults were awaiting inpatient care.
The centers will get Sununu’s reply Feb. 14, when he is expected to release his proposed two-year budget. Should he include their nearly $30 million request, the funding would still face months of budget negotiations between the House and Senate.
Untreated mental illness has been linked to increased risk of other illnesses, substance misuse, homelessness, and incarceration, as well as work and school challenges. Those who go without treatment are also at greater risk of suicide, the second leading cause of death for Granite Staters ages 10 to 14 and 25 to 34, according to the Centers for Disease Control and Prevention.
The pandemic exacerbated barriers to mental health treatment, triggering more to seek help as many were leaving their jobs. The pandemic also brought the state significant money to address the treatment shortages.
With Sununu’s endorsement, the Department of Health and Human Services spent $15 million to buy Hampstead Hospital to expand in- and out-patient treatment for children and adolescents. A year ago, the state launched its Rapid Response Access Point, a 24/7 call center for people seeking mental health and substance misuse treatment. It can be reached at 833-710-6477, via the national hotline number, 988, or online at nh988.com. Leon said in its first year, the call center responded to nearly 22,000 calls, texts, or chat messages.
All 10 community mental health centers now have mobile crisis response teams that respond to a person’s location, giving them an alternative to the emergency room. In the first six months of 2022, the teams made nearly 8,400 stabilization visits.
Leon said the department is renovating a 15-bed unit at Hampstead Hospital that will serve children and adolescents. It has also expanded its treatment teams to include nurses, mental health counselors with bachelor degrees, and counselor aides to reach more kids.
The centers received funding in the last budget to begin expanding step-down housing in their communities. And they used nearly $45 million in federal pandemic aid for staff bonuses, salary adjustments, benefits, and training with hopes the investments would encourage staff to stay and bring in new hires.
At Riverbend Community Mental Health in Concord, staff received gift cards, new desk chairs, and wellness activities. Particularly popular was the car detailing offered to staff who work outside the office, visiting clients in the community.
“It was a huge hit to the point where we’re looking to see if we can do it again,” said Lisa Madden, Riverbend’s chief executive officer. “They felt like they were honored and respected that they do their work in their car.”

Susan Stearns, executive director of NAMI NH, which connects families with support and resources but does not provide treatment, said those investments, particularly the call center, are a meaningful step forward.
“I realize that there’s still more work to be done there in building that system out,” she said. “But that gives me great hope. When I think this is so big and so challenging, I think New Hampshire was able to, in the midst of a pandemic, stand up this truly transformational systems change. So, we know we can do hard things. I take real hope out of things like that. It’s just that the need is so great.”
Stearns knows families, providers, and advocates are frustrated the investments have not eliminated the barriers to treatment.
“I don’t mean that they’re taking longer than one would expect because systems take time to transform,” she said. “We don’t have a lot of time is the problem.”
Center leaders say addressing that need cannot be done without overcoming a paralyzing workforce shortage. They say that can’t be done without an annual increase of $26 million to $28 million for salary increases. In addition, Madden said the student loan forgiveness available to clinicians with masters degrees must be expanded to bachelor-level clinicians.
Madden is trying to fill 40 vacancies, 37 of them clinical jobs working directly with patients. Turnover is particularly high for new employees, she said. Forty-five percent of people left their jobs within their first year and 22 percent in between one and two years.
Like Madden, Pritchard said job postings sometimes run for weeks with no response.
“In the old days, if you had a higher demand, you just hired more staff,” Pritchard said. “Now, there’s no one to bring in the door.” Instead, she said, clinical staff are trying to meet increased demand by taking on additional clients or extending time between clients’ appointments.
Lamy said that’s allowed centers to see more clients even as the number of clinical staff have declined, but also increases the risk of staff burnout.
“I’ve been doing this for a long time, and the sadness that you can see on providers’ faces knowing that we can’t meet the demand, not from a lack of effort, not from lack of desire,” Madden said. “It is real. It really chips away at the core of your professional being, and it’s a tough thing to watch.”
It’s painful for clients, too.

“There’s no question that the thing we get calls (about) most often is that difficulty accessing care, getting that initial appointment,” Stearns said. “If you’re lucky, you talk to someone who says we can put you on a waitlist. Some places will say, ‘Call back every day until we have an opening.’ Some say, ‘We don’t think we’re going to have an opening anytime in the future that we can predict.’ ”
A Concord mother and her 15-year-old son, who asked they not be named to protect his privacy, have been hit particularly hard by the workforce shortage.
He has been in Concord Hospital’s emergency room since Jan. 6, awaiting one of 55 beds at Hampstead Hospital, the only in-patient care for children in the state. He wasn’t alone.
On Monday, 11 additional kids were awaiting a bed. Staff shortages were partly to blame for the 55 adults and children waiting for admission. Nine of Hampstead Hospital beds are closed because of staff vacancies, Leon said. New Hampshire Hospital, the largest behavioral health hospital in the state for adults, is down 31 beds for the same reason, leaving about 150 available, he said.
The 15-year-old’s mother said his wait is longer than most because the hospital requires him to have a single room. He was first hospitalized at Hampstead last summer following an amphetamine psychosis triggered by ADHD medication.
She said he became belligerent and angry, both out of character for him. Deep anxiety followed. “It’s really kind of scary,” the woman said. He began counseling after waiting a year for an opening at Riverbend, she said.
Her son called 911 on Jan. 6, saying he was afraid he was going to hurt himself. He went to Concord Hospital that day.
The holding area, called the “yellow pod,” is not intended to hold someone for days, much less weeks. The boy’s mother said he did not receive his prescribed medication until several days after arriving and is monitored by people without training in mental illness. “They don’t know how to de-escalate,” she said. “The smallest thing becomes the biggest thing.”
Yet her son has not asked to be discharged, she said.
“He has come to grips with the fact that this is a means to an end and that this is something that he has to do. He knows the system is broken. I feel like he understands that.”
This story was originally published by New Hampshire Bulletin.
This article originally appeared on Portsmouth Herald: NH mental health centers in crisis seek help: ‘System is broken’

