TennCare begins reviewing eligibility of beneficiaries this month
Nearly 85,000 Tennesseans are having their eligibility for TennCare services reviewed this month, the first such audit of state Medicaid services since the federal government ended its pandemic-related public health emergency.
TennCare was able to auto-renew more than 30% of the 84,979 residents up for renewal this month, said spokeswoman Amy Lawrence. For the rest, the agency is sending out packets for people to confirm whether they meet financial requirements.
More than 350,000 Tennesseans could ultimately lose coverage after the state completes its process of redetermining the eligibility of beneficiaries in stages during the coming months, according to state estimates. That's roughly one-fifth of the 1.75 million Tennesseans expected to be covered by the program later this year.
Advocates for the under-insured are keeping a close eye on the redetermination process. TennCare was also sued several years ago after hundreds of thousands of residents faced the possibility of losing their coverage because of the then-cumbersome process of verifying eligibility through hard-copy forms and the mail.
Related coverage: At least 220,000 Tennessee kids faced loss of health insurance due to lacking paperwork
More: More than 350,000 Tennesseans could lose TennCare coverage early next year, experts warn
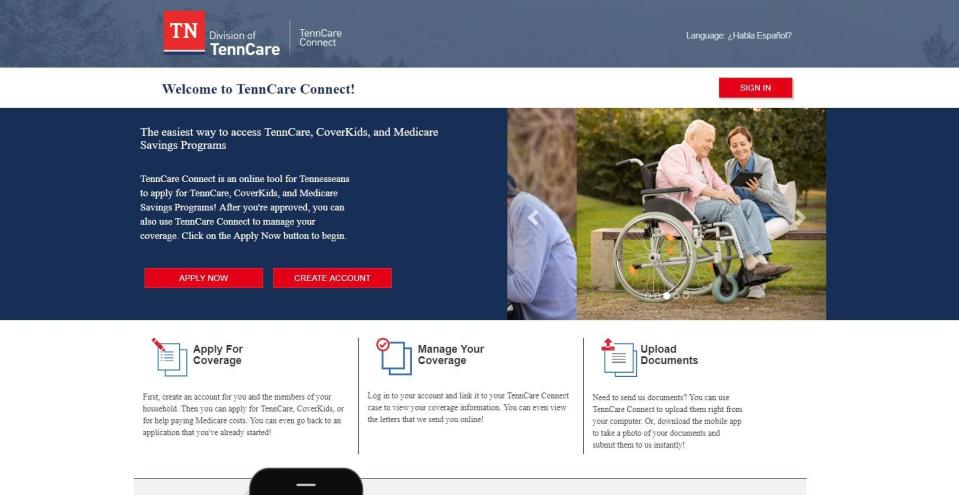
TennCare has since launched an online portal for beneficiaries to confirm their contact information at tenncareconnect.tn.gov. Beneficiaries may also call 855-259-0701. TennCare officials say residents should also make sure to open and respond to any mail they receive from the agency.
"While we’re still fairly early on in the process, it has been smooth thus far," Lawrence said." We will continue to monitor for any problems."
The Tennessee Justice Center, a non-profit advocacy group, is helping people retain their coverage and is suing the state over the way it determines who is eligible. Michele Johnson, the organization's executive director, said the online portal helps but the state is still not doing enough to help many beneficiaries who are elderly, homeless, disabled or who don't speak English.
Redetermination packets are now out and we're happy to help! Luke, one of our client advocates, has completed his first renewals and is ready to help you with yours!
The renewal process will be a long one, so keep an eye out over the next few months for your packet! pic.twitter.com/wghf8EQPjg— Tennessee Justice Center (@TNJusticeCenter) April 13, 2023
"They still might disenroll people inappropriately. And they still haven't fixed this issue of making it accessible for people with disabilities and older Tennesseans," Johnson said. "But the fact that you can actually look online and see the status of your application is an improvement. Most of the clients we serve, especially older folks, they don't have access to either wifi or the technology or understand the technology well enough to navigate that system. But if they call us, we can help them navigate it."
TennCare began mailing out 30,000 renewal packets to households earlier this month. More will go out in the weeks and months ahead. For more information on completing a renewal packet, people can visit tn.gov/tcrenew. TennCare has also created flyers for community organizations to download by visiting TN.gov/tenncare/renewals.
Frank Gluck is the health care reporter for The Tennessean. He can be reached at fgluck@tennessean.com. Follow him on Twitter at @FrankGluck.
Want to read more stories like this? A subscription to one of our Tennessee publications gets you unlimited access to all the latest political news, plus newsletters, a personalized mobile experience, and the ability to tap into stories, photos and videos from throughout the USA TODAY Network's daily sites.
This article originally appeared on Nashville Tennessean: TennCare begins eligibility review for almost 85K beneficiaries
