Test to Treat: pharmacists say Biden’s major new Covid initiative won’t work
A major new Biden administration initiative to facilitate access to Covid-19 antivirals will have a limited impact and fail to mitigate certain health inequities, major pharmacist groups argue, because pharmacists are restricted from prescribing the pills.
Announced in Joe Biden’s State of the Union address, the “Test to Treat” program is meant to address the maddening difficulty Americans have had in accessing Covid-19 treatments. The administration will channel newly increasing stocks of antiviral pills to major retail pharmacies that have in-house clinics, providing one-stop testing and antivirals access.
The program, which the administration aims to provide for free (in the face of fierce Republican opposition to new Covid-19 spending), is also slated to roll out in Veterans Affairs clinics, community health centers and long-term care facilities.
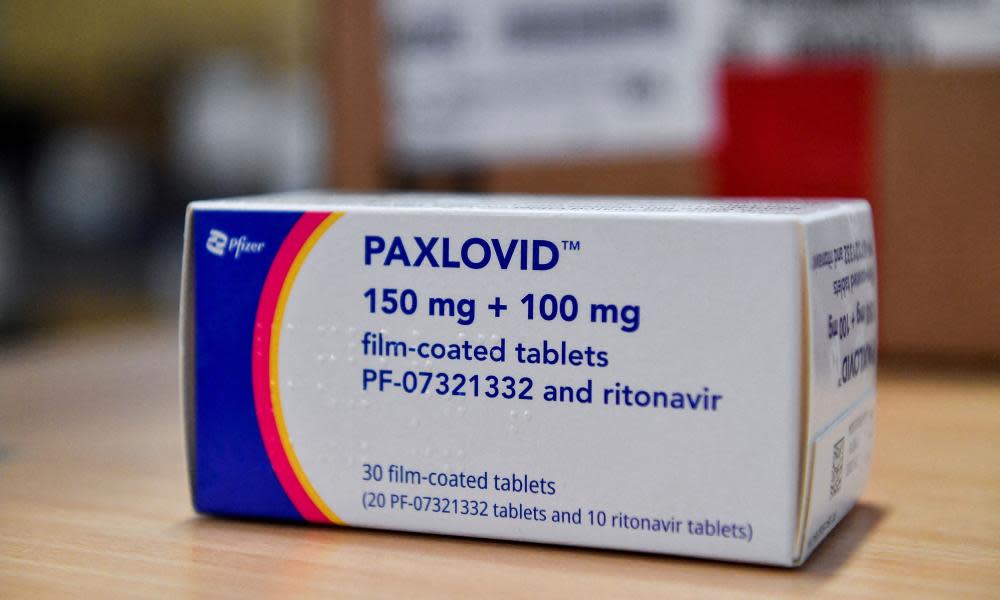
Major participants include some 250 Walgreens stores, 225 Kroger Little Clinics and 1,200 CVS MinuteClinics. CVS clinics in particular are staffed by nurse practitioners and physician assistants, authorized by the Food and Drug Administration (FDA) to prescribe the two currently available Covid antivirals, Pfizer’s Paxlovid and Merck and Ridgeback Biotherapeutics’ molnupiravir.
In a 9 March letter to Biden calling for pharmacists to be granted authority to prescribe these pills, 14 organizations representing pharmacies and pharmacists insisted Test to Treat’s impact will be compromised by the fact that such in-house clinics are relatively limited in number and largely in urban areas.
“Unfortunately, rural and underserved communities are less likely to benefit from your test to treat approach because of this limitation,” the letter states.
According to the Centers for Disease Control and Prevention (CDC), 90% of Americans live within five miles of one of approximately 60,000 pharmacies.
“The FDA is still blocking us from leveraging the most accessible healthcare provider out there to make sure that these patients can get these drugs easily,” said Michael Ganio, a Columbus, Ohio pharmacist, senior director of pharmacy practice and quality at the American Society of Health-System Pharmacists, which is a signatory of the letter to Biden.
“As far as expanding access,” said Ganio, Test to Treat is “not doing a lot”.
The need for Covid-19 antivirals is likely to be greater in rural areas, at least on a per-capita basis. A recent CDC study found that through January, 58.5% of people aged five and older in rural counties had received at least one coronavirus vaccination shot, compared with 75.4% in urban counties.
Paxlovid and molnupiravir are authorized for individuals at high risk of severe Covid-19, in particular unvaccinated people with certain medical conditions. Paxlovid was 88% effective at preventing hospitalization and death in its clinical trial. Molnupiravir proved just 30% effective. The FDA only authorizes its use when other treatments are unavailable or aren’t advised for an individual.
Sufficient supply of Paxlovid will be key to Test to Treat. Since late December, the federal government has delivered a woefully inadequate 700,000 Paxlovid courses to states, the biweekly allotment increasing from 100,000 in January to 175,000 in March.
The administration has claimed it will distribute 1m courses in March and 2.5m in April. A Pfizer representative would only state that the company plans to deliver a cumulative 10m courses by the end of June. The administration has agreed to purchase 20m courses, slated to be delivered by the end of September.
In September 2021, the US Department of Health and Human Services amended a federal public health emergency law, the Prep Act, to grant licensed pharmacists the authority “to order and administer select Covid-19 therapeutics” – which at the time meant monoclonal antibodies and vaccines.
But when the FDA authorized Paxlovid and molnupiravir in December, it explicitly restricted pharmacists from prescribing them.
Authors of the letter to Biden say they submitted data to the FDA at the end of January, hoping to persuade it to grant pharmacists prescribing authority.
These groups have also lobbied the federal government to ensure Medicare Part B would reimburse pharmacists for such prescribing – a move that would probably lead health insurers to follow.
Prescribing Paxlovid safely can be challenging, because it may interact harmfully with other medications. Additionally, the FDA advises against providing the treatment to those with severe kidney or liver impairment. Experts have also raised concerns about molnupiravir’s potential toxicities. It cannot be prescribed to minors and is not advised for pregnant women.
Chanapa Tantibanchachai, an FDA press officer, said the agency’s decision to forbid pharmacists from prescribing Paxlovid and molnupiravir “was based on several factors, including the drugs’ side-effect profiles, the need to assess potential for drug interactions, the need to assess potential kidney function problems (including the severity of potential problems), and the need to evaluate patients for pre-existing conditions” linked to severe Covid-19.
Tantibanchachai said the FDA could revise the policy “as new data and information become available”.
On 4 March, the American Medical Association said the “pharmacy based clinic component of the Test to Treat plan flaunts patient safety and risks significant negative health outcomes”. The AMA argued that by prescribing Covid antivirals at such clinics, providers may endanger patients for whom they lack a comprehensive medical history.
The pharmacy groups insisted in their letter to Biden they have the expertise to prescribe these medications.
In an email to the Guardian, Al Carter, executive director of the National Association of Boards of Pharmacy, stated: “Pharmacists have more complete access to the patients’ medication in comparison to physicians, especially since most patients have more than one prescriber, who don’t necessarily talk with each other.
“Pharmacists spend their whole education focused on medications and their impacts on the body; whereas physicians take the minimal number of classes on pharmacology.”
Katherine Yang, a clinical pharmacist at the University of California, San Francisco, said: “There are a lot of studies that show that when you increase services in community pharmacies, you improve care. In a lot of neighborhoods and rural areas, people may not have access to primary care, and pharmacists are the most accessible public health provider the patients can see.”

