Texas Democrats send letter to federal agency over state dropping people from Medicaid

- Oops!Something went wrong.Please try again later.
Two emails from whistleblowers at the Texas Health and Human Services Commission concerning Texans being disenrolled from Medicaid coverage have drawn the attention of Texas members of the U.S. House.
A letter from Texas Democrats states that almost 600,000 Texans have had their health coverage terminated in the past four months, 81% of the people who have undergone the reevaluation process for Medicaid. Those numbers are based on a June report by the Texas Health and Human Services Commission.
Democratic Reps. Lloyd Doggett, Greg Casar, Joaquin Castro, Colin Allred, Jasmine Crockett, Veronica Escobar, Henry Cuellar and Lizzie Fletcher sent a letter Tuesday to the Centers for Medicare & Medicaid Services, the federal agency that oversees Medicaid, asking Administrator Chiquita Brooks-LaSure to "ensure State compliance with federal rules."
Doggett said he expected to meet with the center later Thursday.
"We've had concerns about it throughout," Doggett said of the Medicaid disenrollment process.
Medicaid in Texas is available for pregnant people and for children based on income. For a family of four, the income is less than $3,083 a month. For a pregnant woman with a family of four it is less than $4,579 a month.
Investigation: How the Austin American-Statesman unearthed crisis and violence in the Texas Medicaid waiver system.
Texas Health and Human Services spokesperson Tiffany Young said the agency is working with partners to ensure the redetermination process operates smoothly.
"Texas is currently in compliance with CMS unwind requirements," she said.
The state reminds: "Clients may lose coverage if they do not respond timely to HHSC mailings. These denials are not erroneous, HHSC urges all clients to respond to any letter received as soon as possible."
On the current state dashboard, 490,723 people have been denied coverage for procedural reasons like not answering letters and 125,831 people have been dropped because they are ineligible for coverage. The state has approved 242,717. More than 5 million people still need to be assessed.
Of the cohorts of people it has reached out to for reenrollment, the state has denied 67%, approved 26% and 7% are pending determination.

What do the whistleblower letters say?
The whistleblower letters come from Concerned Texans; the email used appears to be from a group of state Health and Human Services employees and is addressed to Cecil Young, Texas Health and Human Services executive commissioner.
The American-Statesman reached out to that email address and received no response. Doggett said he did not know the individuals behind the letters.
The allegations in the emails dated July 25 and Aug. 21 include:
In April, the staff received notice that 80,000 people "lost coverage erroneously." That included people who were pregnant, had recently been pregnant, and people in the breast and cervical cancer program.
During the three-year pandemic public health emergency, some newborns lost health coverage due to what parents were told was a "system glitch." Newborns receive 12 months of continuous Medicaid coverage, even not during a pandemic.
In May, 68,000 individuals erroneously lost coverage. "Once again, this action stands in direct contradiction of CMS compliance guidelines," the letter states. Those individuals were eventually reinstated Aug. 5, the letter says.
In the first cohort of people being requalified for Medicaid, more than 5,800 pregnant women lost coverage. Pregnant women receive Medicaid coverage through the first 60 days after birth. On Sept. 1, a new state law will provide women with Medicaid coverage for 12 months after giving birth. That law is not expected to be enacted until CMS approves Texas' plan, which is anticipated early next year.
The current system causing pregnant women to lose coverage was not fixed for a second cohort of people being requalified for Medicaid or for a third cohort, which face it happening to them next month.
A system coding error failed to claim $100 million in federal matching funds because children who qualified for Medicaid were put in the wrong coverage group, the whistleblower email states.
‘They’re waiting for people to die’: Texas’ decadelong waitlists for disability services are getting longer and dangerous
What are the Centers for Medicare & Medicaid Services doing?
CMS has responded to the whistleblowers' emails. Earlier this month, CMS worked with the state to reinstate more than 90,000 people disenrolled erroneously, a CMS spokesperson said.
The state said of the 95,479 people who lost coverage, 1,974 still lack coverage, and 744 of those will have benefits reinstated by the end of the month.
"The technical issues identified have impacted a small fraction of the redeterminations initiated since April," the state said.
CMS said all states received letters on Aug. 9 alerting them to concerns CMS had about the reenrollment process. Texas' letter from CMS noted that in May, 52% of beneficiaries going through the renewal process were disenrolled, typically when someone didn't respond to reenrollment letters.
"This high percent raises concerns that eligible individuals, including children, may be losing coverage," the CMS letter to Texas stated.
A CMS spokesperson said Texas is of concern to CMS. "Because of the size of Medicaid population, the fact that the state hasn't expanded Medicaid, ... there are lots of reasons to be concerned about Texas."
CMS hasn't taken corrective actions against any state, but a CMS spokesperson said it has "levers" it could use. Those include pulling federal funding, requiring a pause in terminations or reenrolling people who have been disenrolled and creating a corrective action plan.
Here are their stories: Vulnerable Texas families wait years for medical care
Why is the Medicaid disenrollment happening?
In Texas, about 2.7 million people have had to requalify for Medicaid benefits after the end of the pandemic emergency in May. Before that, states kept people enrolled throughout the pandemic without having to verify that people still qualified for benefits.
Texas divided Medicaid recipients into cohorts and prioritized for disenrollment people who were likely to no longer qualify for Medicaid because they had aged out or were well past their pregnancy.
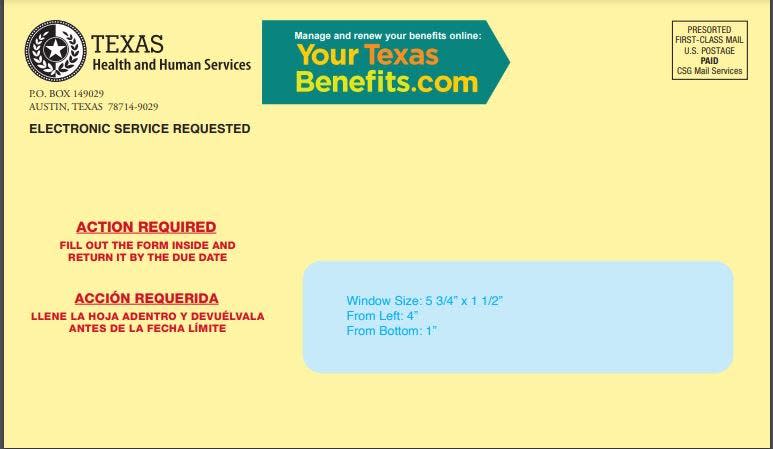
The state has been sending letters in yellow envelopes with red letters "Action Required" to verify that a person qualifies for Medicaid. People have 30 days to complete the reverification process once they receive the envelope.
The information is confusing, though. On the YourTexasBenefits.com website, where people can review their information, the site says this about the Action Required envelopes: "You might receive an envelope that says to return the form inside. There might not be a form included, but you should review the contents and take any action required."
How to: Is my child going to lose Medicaid? What families need to do now to avoid being dropped
How is the Medicaid reenrollment process for people with Medicaid?
The Children's Defense Fund, a nonprofit that advocates for children's issues, responded to that June report:
“We have been sounding the alarm for over a year, urging the state to come up with a methodical, strategic plan to avoid massive Medicaid losses of eligible Texans,” said Adrienne Lloyd, health policy manager at Children’s Defense Fund-Texas, in a press release.
The Statesman contacted local health care communities that serve people receiving Medicaid. Lindsey Tippit, Lone Star Circle of Care chief operations officer, said the federally qualified health center is "not aware of our patients losing Medicaid erroneously."
People's Community Clinic, another federally qualified health center, said many of its clients are women and children and scheduled for enrollment reverification in the fall, making it too early to feel an impact.
Insurance companies that serve Medicaid clients are working to keep people enrolled.
"We always have challenges finding people especially with populations we serve," said Greg Thompson, president of Amerigroup Texas, which offers Medicaid plans. "They may have a new cellphone or a new address that might not be on the state's file."
This article originally appeared on Austin American-Statesman: U.S. Congress now involved over Texas dropping people from Medicaid

