'You think you're free, then it comes back': Doctors and patients explain what the coronavirus 'second-week crash' feels like

Aria Bendix/Business Insider
Some coronavirus patients and the doctors treating them have reported a "second-week crash" in which patients believe they're recovering but then feel much worse.
Second-week crash symptoms include shortness of breath and aches, according to those who have experienced them firsthand.
Related Video: What Could Be the Fastest Way to End the Coronavirus Crisis?
People around the world are publicly sharing their coronavirus symptoms.
These anecdotal reports illustrate that symptoms vary from person to person. One relatively common experience is a second-week crash, where patients felt like they were on the mend, and then in the second week of their illness, their symptoms ramped up and become worse than before.
Health experts are unsure why only a subset of the population has this second-week crash, which often results in a high fever, shortness of breath, and extreme fatigue.
Below, four coronavirus patients and two doctors detail what a second-week crash can feel like.
Aria Bendix, a 27-year-old science journalist, developed excruciating rib-cage pain as she entered her second week of coronavirus symptoms.

In an essay she wrote for Business Insider, Bendix said her mild coronavirus symptoms morphed into more serious ones a week into feeling ill.
Bendix said she initially just had body aches, but 24 hours later she also started to have chills.
"It felt as if I had run a marathon, then been hit by a car. I decided to self-isolate inside my apartment," Bendix wrote.
A few days passed, and Bendix said her aches started to dissipate. She assumed she was on the road to recovery. But then the rib-cage pain started.
"There was a pressure, too — as if someone were squeezing my lungs like an accordion. My breathing felt heavy," Bendix wrote.
After a trip to the emergency room, doctors said they were unable to test Bendix, but that her symptoms signaled she had COVID-19.
Back at home, Bendix said she had a week of sleepless nights and days when breathing was difficult. It wasn't until that week was over that she started to feel normal again.
"That was about the same time I developed a sore throat. For roughly 24 hours, I struggled to swallow food or liquid," Bendix wrote. "By day 14 of my symptoms — the day I was supposed to no longer be contagious — the aches returned. I felt as if I was back to square one, but at least I could breathe."
On April 5, the day Bendix published her essay, she said she started to finally feel more like herself but still had lingering symptoms like a sore throat and fatigue.
Rosemary O'Hara, an editor at the South Florida Sun Sentinel, said she felt like she needed an oxygen mask during her second week of symptoms.

In her March 17 essay in the South Florida Sun Sentinel, O'Hara said that a day after beginning to feel ill, she developed a fever, cough, and shortness of breath.
"At the urgent care center, the doctor diagnosed pneumonia," O'Hara said. She was given antibiotics and after taking them for 10 days, began to feel better.
But then she felt worse.
"Until now, the only time I ever remember paying such close attention to my breathing was when I tried meditation and yoga," O'Hara said. "But one night this past week, my breathing was so labored, it was all I could hear. I felt like I needed an oxygen mask."
O'Hara said she was able to get a test two weeks into feeling ill, and days later it came back negative. But O'Hara was skeptical of that result because it could've meant she didn't have a detectable amount of the virus in her system, she wrote.
"The doctor told me that it's impossible to know if I had the virus because an antibody test is not yet available, so we'll never know for sure," O'Hara wrote, adding that she believes she was one of Florida's first coronavirus patients.
O'Hara didn't share how she's been faring since her emergency room appointment and COVID-19 test experience.
Susan Kane said it was shocking to watch her husband's dry cough transform into serious illness in a matter of days.

Kane, a resident of Snohomish County, Washington, told CBS News that her 55-year-old husband Chris was a non-smoker with no underlying conditions, so it was surprising to see his health deteriorate.
"It started off as just a little bit of a dry cough. He didn't have any other symptoms but this crazy cough," Kane said, but a few days later, "it ramped up, and then it was coughing and choking and just gasping for air."
A week following these symptoms, Chris was finally diagnosed with COVID-19 and given oxygen to help him breathe. Now, Chris is fully recovered.
John Craven, a 41-year-old political reporter, said that based on his experience, the coronavirus 'tricks you' into feeling better and then symptoms like fever and dizziness come back.

"It tricks you," Craven said. "You think you're free, then it comes back."
Craven, who lives and works in New York City, told the Hartford Courant that his coronavirus symptoms began as body aches, dizziness, and shortness of breath for five days.
On the fifth day, Craven said he began to feel better and even did a home workout, but just a few hours later he felt just as sick as he had the days prior.
"It's unpredictable," Craven said of his experience.
His second-week crash symptoms included a fever and dizziness.
"It tricks you," Craven said. "You think you're free, then it comes back."
Craven said he was unable to get tested but believes he had COVID-19.
As of April 2, over two weeks after Craven first felt ill, he said finally started to feel better.
Michelle Gong, the director of critical-care research at Montefiore Medical Center in New York CIty, said that respiratory failure tends to kick in 7 days after symptoms start.
During a Q&A with the Journal of the American Medical Association, Gong said that COVID-19 patients often seem to be "doing OK, and then at around the five- to seven-day mark they start to get worse and then develop respiratory failure."
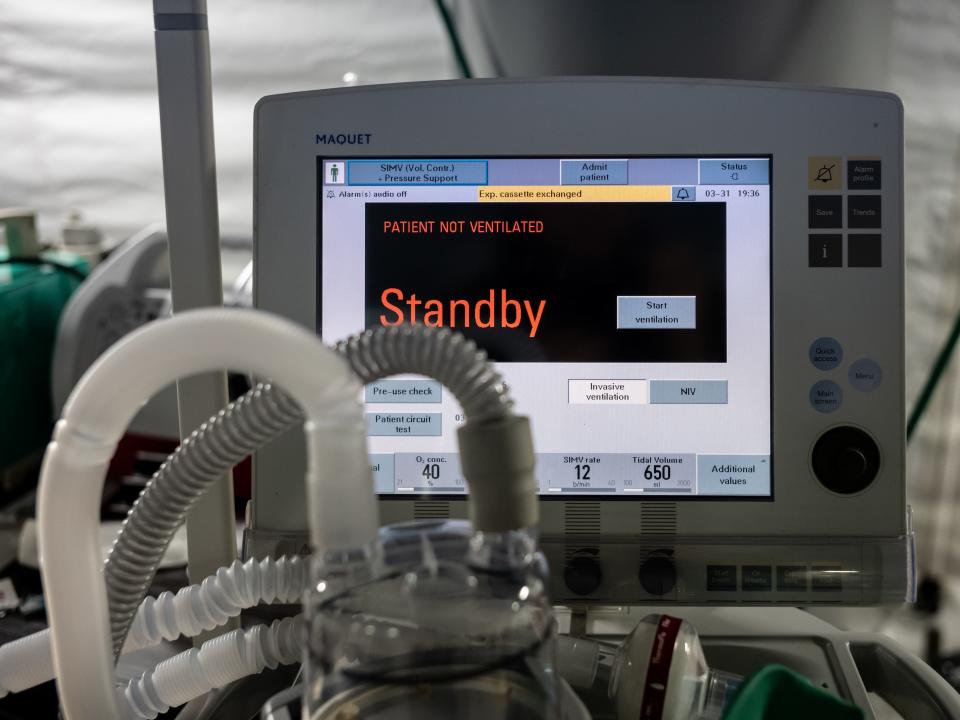
Respiratory failure occurs when the coronavirus attacks your lung's cells and linings and makes oxygen flow throughout the body difficult or impossible. As a result, people in respiratory failure need ventilators to assist their breathing.
Gong added that this shift to more severe symptoms can be "abrupt."
Dr. Christopher Ohl, an infectious disease expert in North Carolina, said he's noticed a rapid decline in health for many patients.

"They say, 'Hey, you know, I think I'm getting over this,' and then within 20 to 24 hours, they've got fevers, severe fatigue, worsening cough and shortness of breath. Then they get hospitalized," Ohl told CBS News of the second-week crash phenomenon.
Read the original article on Business Insider

