Those trendy continuous glucose monitors? I’ve been wearing them for more than a decade. Here’s what I’ve learned
A woman rises slinkily from a hot tub—her long, wet hair glistening in the sunlight, a picturesque sunrise before her—and a continuous glucose monitor perfectly centered on the back of her flawless right arm.
It’s a scene from an ad for one of those trendy continuous glucose monitors (also known as a CGM) that recently popped up in my social feed.
It doesn’t even slightly resemble my life with a CGM—and I should know what that life is like. I’ve been a type 1 diabetic for a quarter century, since I was 12. And I’ve worn a variety of CGM products for more than a decade, from relatively large sensors “stapled” into my stomach to pill-sized sensors implanted under the skin of my upper arm.
And let me tell you, it’s not a glamorous life.
In the latest health wearable trend, manufacturers of technology developed to help diabetics—by warning of potentially deadly high and low glucose episodes—are now marketing their products to non-diabetics. Their pitch: A sensor inserted between layers of skin via a spring-loaded needle will offer metabolism insights that may lead to changes in diet and exercise.
Don’t get me wrong—I’m insanely grateful for CGM technology. It’s grown so much over the past handful of years, from an anxiety-inducing nuisance that constantly throws false alarms, to truly life-saving technology that almost always reliably warns me of impending high and low glucose levels.
But I look nothing like the model. After years of shooting CGMs into the back of my upper arms (as well as injecting insulin and inserting insulin pump and pod infusion sites there), mine are marred and bruised—to the extent that I’m occasionally asked if I’m safe at home.
And a long soak in a hot tub? That’s a no-go (or a “proceed with extreme caution”) for me, as someone for whom a CGM is medically necessary. Diabetics are warned to be extremely careful in hot tubs, since the heat can induce hypoglycemic unawareness that prevents the usual warning signs of low blood sugar levels, like shakiness and sweats.
You would hope my CGM would alert me to a low glucose episode but—as I know first hand from attempts at long, hot baths—they tend to stop reading once submerged for a while. (I spend more time silencing “lost signal” alarms than truly relaxing.)
If you’re relying on reads from your CGM, be wary of extended time in the water—that’s one lesson I’ve learned from over a decade of CGM-wearing. Here are a few others.
1. CGMs don’t measure blood sugar.
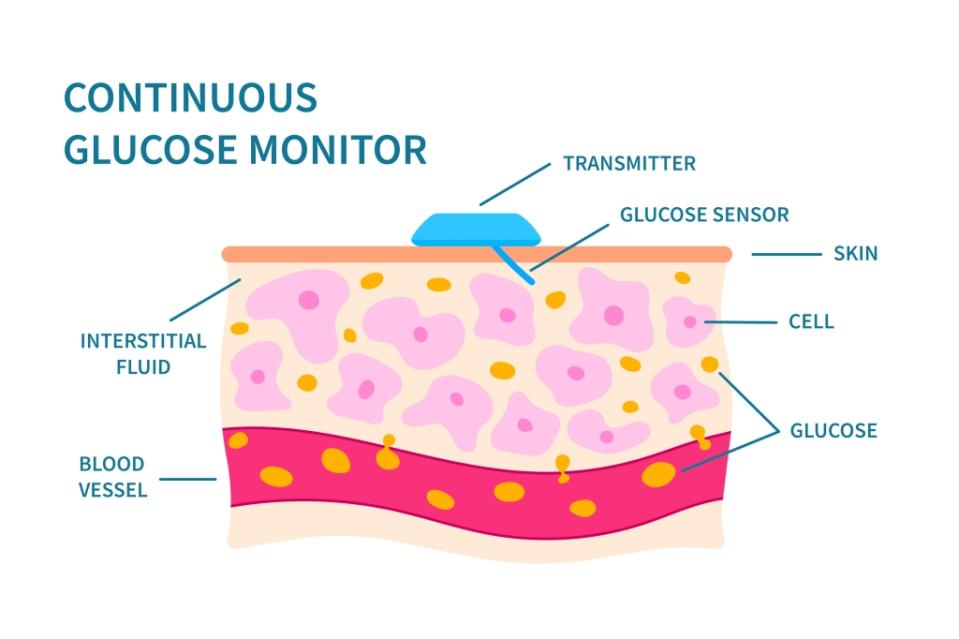
Yep, you read that right. And yep, a bunch of people are saying it wrong—even some of the so-called “pros.” CGMs don’t measure blood glucose levels. They measure glucose in interstitial fluid, between layers of tissue. Glucose tends to flow from blood vessels to the tissue surrounding them. Interstitial fluid glucose levels are similar to blood glucose levels, but lag them by a good 15 minutes or so.
To a non-diabetic, the lag doesn’t make a difference. To a diabetic, it can mean a delay in alert of a low glucose level and, thus, treatment.

2. Food and exercise aren’t the only factors that impact your glucose levels.
CGMs are being marketed to non-diabetics as a tool that allows them to observe the impact of foods on their glucose levels. But plenty of other factors can impact those levels, from illness and certain medications to stress, lack of sleep, and menstrual cycles. I once went into a very contentious meeting with my son’s school with a fairly normal blood glucose level, and left irate—and with a reading in the 400s. (The meeting didn’t go well, to say the least.)

3. Sensors are easy to wear for a week or two—and much harder to wear for longer than that.
Some companies are marketing CGMs to non-diabetics as a temporary inconvenience. Wear a sensor for two weeks and gain data on how food impacts your glucose levels valid for an entire year, they claim.
But such a scenario doesn’t apply to diabetics, especially ones with hypoglycemic unawareness.
The longer one has diabetes, the greater the chance of developing the condition, a form of neuropathy that makes a CGM a daily necessity. Don’t get me wrong—I’m incredibly grateful for my CGM. But my arms are visibly damaged—as was my stomach, when I regularly wore them there.
(Regular CGM users are advised to rotate “sites” when they can—arms, legs, stomach, upper buttocks—to preserve “real estate.” Historically, however, some CGMs were only approved for use on the abdomen or upper buttocks, the later of which can’t be reached without help. And, not all sites work well for all diabetics.)

4. CGMs can ease the “cognitive burden” of diabetics—but they may have the opposite effect for non-diabetics.
It’s been estimated that type 1 diabetics make around 180 health-related decisions a day in an effort to keep their glucose and ketone levels in check. The medical term for this: “cognitive burden.”
When I was young, sometimes my dad would sit up on a Saturday morning and monitor my glucose levels using a traditional blood-based monitor, so I could catch some extra sleep. Wearing a CGM is a bit like having that level of help—but even better, and all the time. It allows me to shift more of my focus elsewhere, knowing that something is keeping an eye on things. It helps shoulder that cognitive burden.
For non-diabetics, however, CGMs could have an opposite effect. Unless you have hypoglycemia, pre-diabetes, or another health condition that puts you at risk for high or low blood glucose levels, you may find that a sensor induces a stressful state of information overload. As someone who doesn’t have issues maintaining healthy oxygen saturation or blood pressure levels, I can’t imagine being presented with a constant stream of such data (and attempting to process and interpret relatively small variations). Honestly, such a “tool” would probably send my anxiety through the roof—and I have to wonder if CGMs do the same for at least some non-diabetics.

5. Not everyone has equal access to this potentially life-saving technology—and that’s a problem.
Insulin, insulin pumps, and now CGMs—add them to the list of expensive treatments diabetics need but can’t always afford. For diabetics—especially type 1s—cognitive burden is a thing, but so is the financial burden.
But there’s a documented lack of access to CGMs among racial and ethnic “minorities” that can’t be explained by socioeconomic status alone. According to a study published this year in the medical journal Diabetes Care, use of diabetes technology like insulin pumps and CGMs was more than 20% lower in Black patients when compared to white patients. And according to a 2021 study in a similar journal, less than a third of Black youth had access to insulin pumps and CGMs, while nearly three-quarters of white patients did (40% of Hispanic patients had access).
Among the reasons: provider bias, systemic racism, and (understandable) mistrust of the medical system, the authors of the later study speculate.
To non-diabetics using CGMs, my message is this: Enjoy the new gadget—though insertion can be quite painful, which takes away some of the fun. Use the data to improve your health, if you can. And if you find it’s not everything you’d hoped, consider donating your unused, unexpired CGM sensors to a charity like Insulin For Life, which distributes supplies to diabetics in developing countries.
The device that annoys and disappoints you could save a diabetic’s life.
This story was originally featured on Fortune.com
More from Fortune:
5 side hustles where you may earn over $20,000 per year—all while working from home
ChatGPT helped me make a plan to buy a $500,000 home, but experts warn me it's a bad idea
This is how much money you need to earn annually to comfortably buy a $600,000 home
