They trusted this assisted living to protect their mother. Then came the call on Christmas
The Rufo brothers received clear instructions from their father as he lay dying: Take care of your mother. When the time comes, find a nice facility for her − a place where she’ll be safe.
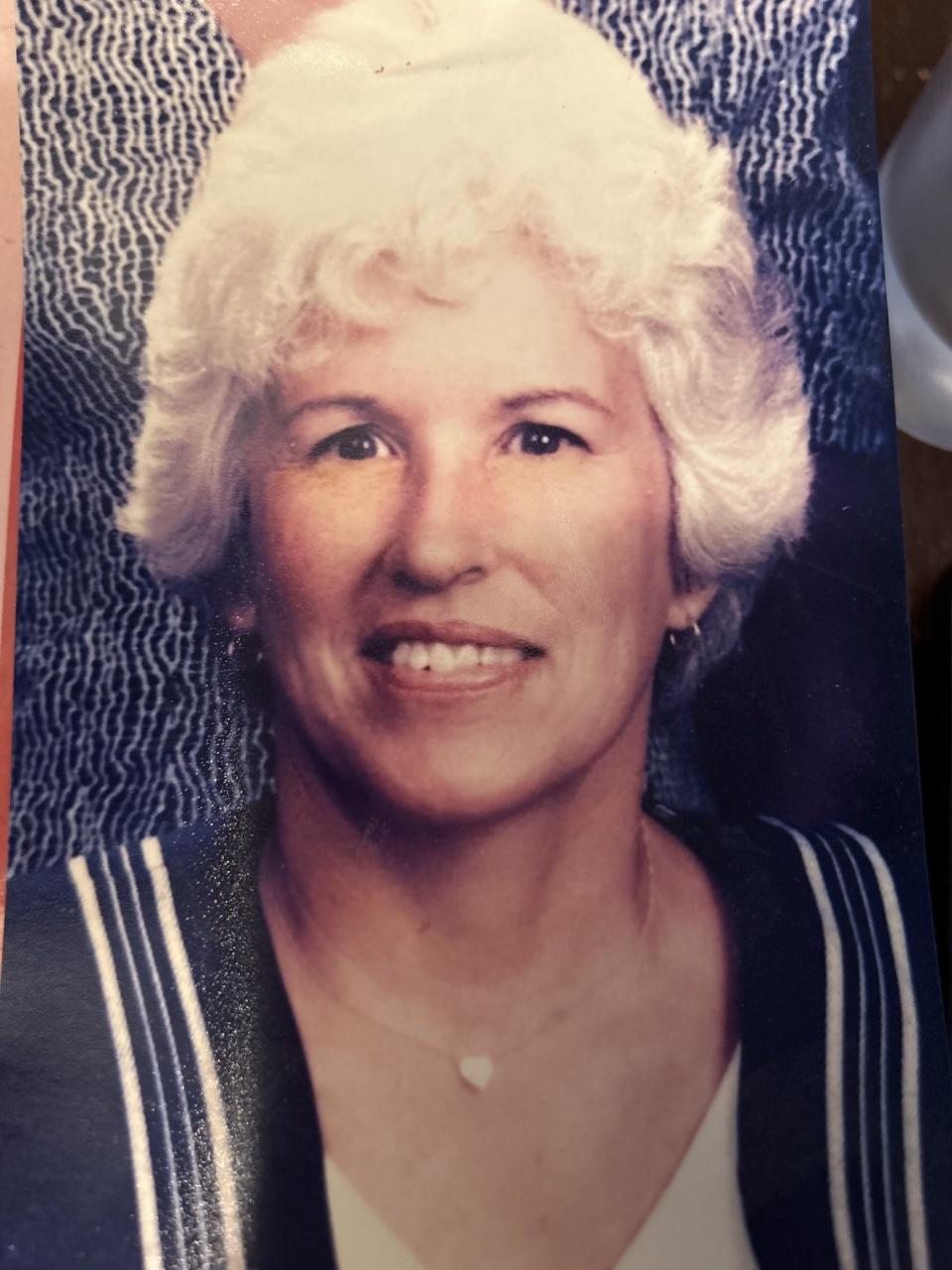
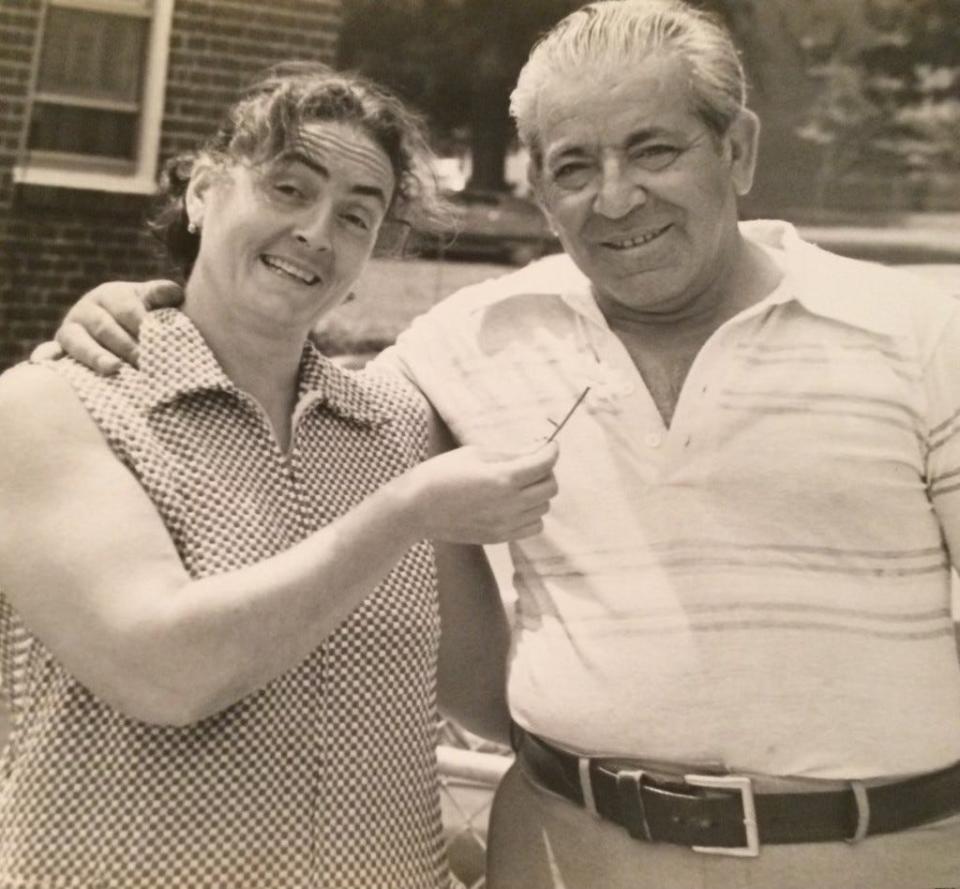
About a decade later in 2020, Maria Rufo no longer remembered how to turn off her gas stovetop. The Italian immigrant and family matriarch’s home, for years, had two fully equipped kitchens: one kept clean for company, the other in the basement where every Christmas Eve Maria cooked the Feast of the Seven Fishes.
Sons Larry and Danny soon divided up morning and night shifts in order to care for Maria – changing, bathing and feeding her. They tried to do her hair as she did.
The fear of Maria falling pushed the family to look into assisted living facilities. Maria moved into Arden Courts, a place that cares for people with dementia, in February 2021.
When Christmas came, the family said the facility advised them to keep Maria at Arden Courts, in Brandywine Hundred, for the holiday. They agreed because they had seen for themselves how she struggled when outside of the facility.
On the late afternoon of Christmas Day 2021, Larry received a phone call from Arden Courts. A resident pushed Maria, breaking her hip. She died one month later.
The Rufo brothers did not know, at that time, that Arden Courts had recorded the highest number of reported abuse incidents of any Delaware assisted living facility in the past decade. Yet the state had, at that point, only investigated Arden Courts four times in the past decade.
The Rufos are among three families who have filed lawsuits against Arden Courts in the past year. All claim abuse and neglect, with another family citing a second instance of resident-to-resident harm.
As Delaware’s population rapidly ages, more residents with dementia are relying on assisted living facilities for care. Unlike nursing homes, assisted living facilities are regulated solely by the state, which results in a weak patchwork of oversight.
Advocates, family caregivers and experts say Arden Courts represents a larger problem of dementia care in the First State. A Delaware Online/News Journal investigation found:
The state has failed to police these types of facilities in the past decade, even as high numbers of abuse, neglect and falls are reported to the Division of Health Care Quality. State surveyors had not inspected many of these assisted living communities for years, according to hundreds of pages of inspection reports from 2013 to 2022. The state has also weakened regulations and continued to underfund the division responsible for oversight.
Three additional families have criticized the quality of care provided by Arden Courts, which once marketed itself as a national leader in dementia care. They say they found their loved ones soaked in urine and severely dehydrated. Arden Courts, some also claim, did not properly handle residents’ injuries, with some being left in severe pain for hours.
The regulations in Delaware, according to experts, former state officials and advocates, are outdated to the current needs of assisting living residents. This wording, experts and advocates say, can be at times vague and likely allows for a wide variability in the types and quality of dementia care these facilities offer.
An Arden Courts spokeswoman declined to comment on a majority of the claims made against the facility, citing residents’ privacy concerns. The News Journal sent detailed questions to the facility outlining the issues raised by family members, which Arden Courts did not answer.

In a statement, the facility said it “strives to create a safe and secure environment for all our residents and is committed to ensuring their emotional and physical well-being.”
“We focus on working closely with residents and families to address any concerns in a timely manner,” the statement reads.
Arden Courts, in legal filings, has denied the claims made in the three lawsuits.
There have been attempts for change: Lawmakers this past session introduced a handful of bills that would have increased dementia training requirements, forbid false marketing and required sufficient staffing for facilities that provide dementia care services. Half of the bills were not voted on.
The industry has also pushed back: Assisted living facilities continue to struggle in a post-pandemic world. It’s hard to recruit staff, especially when other healthcare facilities offer better pay and benefits. The state has failed to fully address its health care workforce shortage for decades.
INVESTIGATIVE REPORTING: She was a geriatric nurse. Why did it take Delaware so long to realize she was neglected?
LeadingAge, a national industry organization that represents long-term care, found in a spring 2023 survey that about 70% of assisted living facilities reported facing a “significant or severe workforce shortage.”
“Resident care is … the number one concern of people who are in this industry,” said Cheryl Heiks, executive director of Delaware Health Care Facilities Association. “But how we get it is very difficult if we don't have enough people and the right people.”
Administrators of long-term care facilities told lawmakers in June that adding more requirements will make it harder to fill vacancies.
A June 2021 inspection report showed Arden Courts struggled with staffing levels. State officials said the incident involving Maria Rufo has been investigated, with Arden Courts not receiving any regulatory deficiencies for it.
ASSISTED LIVING DATABASE: Read inspection reports for all Delaware assisted living facilities
The Rufo brothers, their wives and Maria’s five grandchildren still feel they do not know all of the circumstances that led to the matriarch’s death – or if it could have been prevented.
“I'll never have my mother back,” said Danny Rufo. “My brother and I were charged with a duty to protect my mother and we thought we were. And that's what makes it hurt even more.
“Because I had a responsibility here and look what happened.”
'She fought back'
Every night as a boy, Danny Rufo waited for his mother’s nightly phone call. She worked late into the evening at the family’s pizza shop. She called her youngest son around 11 p.m. just before she walked home.
Danny sat near the window as he waited to spot his mother walking alone on the dark streets outside of Wilmington's Little Italy. He didn’t move out of his parent’s home until his wedding day.
Both he and Larry were raised in a traditional Italian home: Saints were prayed to and superstitions were respected. The brothers, throughout their childhoods, were aware of the emotional and physical pain their mother carried.
Maria was pregnant nine times. Larry and Danny, born 13 years apart, are her only living children. The other pregnancies resulted in miscarriages or stillbirths. For as long as they can remember, their mother had complained of back pain.
“She wasn’t one to fall down easily,” Larry said. “She fought back.”

As they became men, the brothers became even more protective. When dementia made daily life unsafe for Maria, they thought they did due diligence when finding a place: They hired a consultant and virtually toured two different facilities.
What they didn't know when Maria entered Arden Courts in February 2021 was that the facility had been inspected just three times since 2013. For a stretch of five years, no annual or complaint inspections took place – which was not a rarity.
For much of the past decade, the Division of Health Care Quality has not regularly inspected most assisted living facilities, according to News Journal analysis. A majority of these facilities offer some type of dementia or memory care service.
The News Journal submitted a Freedom of Information Act request for all assisted living inspection reports from 2013 to 2022. Hundreds of pages showed how years went by when assisted living facilities, large and small, were not inspected.
The News Journal previously reported that the Division of Health Care Quality has struggled for about a decade to investigate complaints made against long-term care facilities – particularly for assisted living facilities.
The state has chronic issues with hiring and retaining staff to investigate these facilities, in part because of low salaries. The governor’s office has denied the division’s repeated requests for additional funding.
Delaware’s health department is working to fill the vacancies. State officials said there are currently three vacancies among the 21 total positions. Eight surveyors are in the process of completing required training.
Mary Peterson, who worked as DHCQ director from 2013 to 2019, said the division had to “ignore” annual inspections of assisted living facilities in order to get a handle on the incoming complaints and other responsibilities.
But the state also weakened regulations.
The Delaware General Assembly voted in 2018 to change DHCQ’s requirement to inspect long-term care facilities from an “annual” to “regular” basis, empowering the agency to do less frequent inspections.
Peterson said this was done because the division was “so far behind” on surveys and did not “have the resources necessary to do what was the required mission of the division.”
In 2019, the state did the fewest number of inspections since 2013 – a total of four, records show. Yet facilities collectively had the highest number of reported incidences of abuse and falls that year.
When something bad happens in a facility – such as a fall, a case of alleged abuse, a medical error – the assisted living facility is required to report it to the state within eight hours.
The Division of Health Care Quality also receives reported incidents and complaints from residents, families and employees, among other sources.
This data, which consists of substantiated and unsubstantiated incidents, is captured in the state’s referral intake database. Surveys are prioritized “based on a number of factors including the length of time since the last survey, and the triage level of facility reported incidents and complaint intakes,” a health department spokesman said.
The News Journal obtained the referral intake data through a Freedom of Information Act request. Analysis shows that some facilities had high numbers of abuse, neglect and falls even as they were not inspected for years.
Brandywine Assisted Living at Fenwick Island, which has a bed capacity of 125, had the most reported falls of any facility between 2013 to 2021: 1,430. In that time period, it was inspected three times.
Brandywine Assisted Living at Seaside Pointe, which has a bed capacity of 150, had 1,049 reported falls in that same time period. Seaside Pointe was inspected four times – the first time being in December 2019. There were no inspections from 2013 until that year, records show.
One Seaside Pointe resident who had dementia, according to a 2019 inspection report, fell 41 times in eight months. Ten of these falls occurred when the resident was attempting to go to the bathroom.
The state found the facility failed to: reassess this resident “after her falls, to implement a new plan of care and provide care and services to prevent” her from falling again. Falls are the leading cause of injury death among older Americans.
In its plan of correction, the facility said its leadership would meet weekly to review fall interventions, among other changes.
MORE: They thought their mother was safe in her nursing home. Then their worst fear came true
Arden Courts, which has a 56-bed occupancy, saw 214 incidents of reported abuse from 2013 to 2021, the highest of any assisted living facility in that time period.
The facility in its statement said it “tends to take a comprehensive approach, proactively sharing any event in question whether or not state law requires it to be reported.”
“While that high level of transparency facilitates stronger regulatory partnerships, it could result in more incidents being reported by comparison,” the statement reads. Arden Courts did not provide any clarification on what this means and examples of events that have been reported that are not outlined in state law.
The health department did not make anyone from the Division of Health Care Quality leadership available for an interview for this story. The state did provide a statement attributed to DHCQ Director Corinna Getchell, noting she can only speak of the division’s “operations since coming into the position of director in August 2020.” Getchell worked for the division before becoming director.
She said in a written statement that during the pandemic, surveyors only visited facilities for COVID-19 infection control surveys and for “issues being triaged as an immediate jeopardy issue.” Routine surveys began again in 2021, though the division had a limited number of surveyors. The division’s staff triaged complaints and those identified as immediate jeopardy were the priority.
In 2021 and 2022, according to News Journal analysis, more than half of Delaware’s assisted living facilities were not inspected.
'Why did you push me?'
Just one month after Maria Rufo moved in, Arden Courts resident Anita Taylor wandered into another man’s room.
Anita had a tendency to do this, according to the March 22, 2021 incident report. It was a symptom of her dementia. She was often confused by her surroundings – it’s one reason why her son, William Taylor, placed her at Arden Courts.
Suddenly, an Arden Courts employee heard a bang and found Anita on the floor. She then reportedly screamed: “Why did you push me?”
No employees witnessed Anita being pushed, according to an incident report.

William Taylor remembered receiving the phone call when he was at work. An Arden Courts employee said Anita was “severely” injured and already en route to Wilmington Hospital, he recalled.
Of the substantiated and unsubstantiated abuse incidents involving Arden Courts from 2018 to 2021, about 55% involved resident-to-resident harm, according to data The News Journal obtained through a Freedom of Information Act.
Most people with dementia are not aggressive, said Eilon Caspi, a dementia behavioral specialist and professor at the University of Connecticut. Those that are often lash out because they are confused, scared or frustrated and are unable to communicate like they once could.
Many of the circumstances stem from an invasion of personal space or conflicts between roommates, such as someone taking an object they believe belongs to them, he said.
Does your family have an experience with a Delaware assisted living facility? Fill out this form.
Caspi said responsibility should be placed on the facility – not the resident – for this behavior. He attributed understaffing and undertraining as often major contributors.
He published in 2018 the first North American pilot study analyzing resident-to-resident incidences among those with dementia in long-term care facilities. The study found that the majority of the fatal incidents were reported unwitnessed by staff, identifying inadequate supervision as a possible factor.
A 2018 inspection report detailed how inadequate staffing at State Street, in Dover, allowed one resident with dementia to sexually abuse another resident for about two months. It often took place in the common area of the locked memory care unit. For one of these incidents, the common area was unattended despite two staff members being assigned to the unit. The facility disciplined these employees and made subsequent changes to fix its staffing issues.
Previous research, Caspi said, suggests that most incidents are preventable. One U.S. study from 2016 found that higher caseloads among aides in nursing homes were associated with higher incident rates.
A majority of fatal resident-to-resident incidents, he said, involve a push.
When analyzing inspection reports, The News Journal found that five facilities were cited in part for not properly handling resident-to-resident harm. Arden Courts was never cited for this issue or for abuse or neglect in its five inspection reports.
But Milford Place was. It had the third highest number of total abuse incidents reported, according to News Journal analysis.
In a 2019 inspection report, the state found one resident, named R8 in the report, harmed another resident as well as seven “unidentified others” for a period of seven months. R8, who suffered from dementia, pushed others against a wall, threw them to the ground or slapped them.
Each time this occurred, the facility “immediately separated” the residents and ensured that R8 was in constant eyesight of staff for a 72-hour period. Yet the frequent monitoring was not documented. The resident was also sent to the hospital in some cases.
The state surveyor, during the inspection, asked what interventions were set in place. Milford Place did not provide any information. The state official asked if the facility had considered “one on one monitoring.”
The care services manager said a “discussion took place with R8’s responsible party to pay for one on one monitoring services, however, R8’s family did not agree to pay for the service, thus, one on one monitoring was not implemented as an intervention.”
‘She just gave up’
Anita, who golfed, bowled and liked to go on long walks, was never able to regain full function after being pushed. Her family moved her to a skilled nursing facility, where she remained in bed for the remainder of her life.
“She just gave up,” William Taylor said. “She was so full of life prior to that injury. Everything went 180 degrees the other way.”
Taylor died a year later at the age of 74.
In late June 2021, a state surveyor inspected Arden Courts for a complaint filed by William Taylor.
The state official could not substantiate abuse, so Arden Courts was not cited for it. But the complaint summary noted it was the third incident of aggression from the man who pushed Anita, according to the document obtained by The News Journal.
Arden Courts was ultimately cited for not including “measurable goals or specific interventions” regarding two residents, who appear to be Anita and the man who pushed her. In Anita’s service agreement, according to the inspection report, there was no mention of her wandering behavior.
The facility, in its plan of correction, wrote it would do a monthly audit of residents’ service agreements.
The inspection report also details the injuries of resident Dale Houchins. Her family is also suing Arden Courts.
Dale, whose grandchildren and their friends affectionately called her “Ahby,” was mostly nonverbal and required a wheelchair. She could not walk or get herself out of bed.
On June 9, 2021, an Arden Courts caregiver found 82-year-old Houchins in bed with “significant injuries.”
At the hospital, Dale was given fentanyl for her pain. She had a fractured femur, vertebrae and sacrum. Doctors found a slight laceration to the spleen and internal bleeding to the abdominal wall.
Heather Houchins, Dale’s daughter, recalled how a doctor pulled her aside, concerned about how her mother could have gotten this hurt.
While Dale was in surgery, her children decided to go to Arden Courts, hoping to speak with someone about how their mother got injured. The administrator, Heather Houchins said, had “no idea my mom had gone to the hospital.”
Dale was discharged in July and transferred to a Hockessin nursing home. She died in December 2021, with the family claiming in the lawsuit that it was due to her injuries.
Heather Houchins said she and her brother still do not know how their mother was injured. And neither does the facility, according to the June 2021 inspection report.

The report – which does not name Dale, but the incident matches up with the dates and description of the injuries – found that Arden Courts was understaffed the night a resident assistant found Dale.
Three resident assistants and a nurse were working that night, according to the inspection report. Typically, four resident assistants and a nurse staff the night shift, with each resident assistant assigned to one of the four areas of the facility. At the time of the inspection, Arden Courts cared for 44 residents.
Arden Courts, the surveyor also determined, failed to follow the state requirement of staff receiving 12 hours of education. This is supposed to cover issues like “health and psychosocial needs of the population being served,” in addition to infection control, basic first aid and other job responsibilities, according to state regulations. Following the inspection, the facility began training for all of its employees.
The state official looked at records for five resident assistants, all of whom had not reached even one-third of the hours required in annual education.
Two of those employees worked the night shift when Dale’s injuries were discovered.
‘We need this not only for our own peace’
To their surprise, Larry and Danny Rufo found their mother adjusted to Arden Courts. When they stopped by, they often found her in the middle of a group activity. She was once too busy playing group Bingo to spend time with them.
She fell a few times in her first six months there. While some led to trips to the hospital, she had no major injuries.
Christmas 2021 was the first time either Larry or Danny would not spend with their mother. They decided to break it up: Danny brought his wife and children to visit Maria on Christmas Eve. They sang holiday songs in Italian. Danny brought presents for her and other residents. The plan was for Larry and his family to visit the day after Christmas.
Late afternoon on Christmas, Larry received a phone call from Arden Courts. The employee told him Maria had been pushed by another resident. She was complaining of pain and was not able to stand.
He recalled, in an email written the next day and reviewed by The News Journal, that the employee said his mother was not in “serious distress.”
Larry and his wife Melissa, who was present for this conversation and also spoke with Arden Courts officials on Christmas Day, said he was asked if his mother should go to the hospital.
Shouldn’t a doctor make that decision, he recalled thinking.
This was during the rise of the COVID-19 omicron variant. Larry knew his mother did not do well outside of Arden Courts and he also worried about her sitting in an emergency department with COVID-19 rapidly spreading.
Is the hospital necessary, he remembered asking. Can you give her Motrin and ice? The Rufos said they were not given any details about her injury, including that Maria had a fractured hip, until hours later.
Both Larry and Melissa said they did not sense urgency from Arden Courts. They said they called the facility for updates Christmas night and it took a while to get a response.
Arden Courts, in its records obtained by The News Journal, tells a different story.
Mavis Cromwell, an Arden Courts licensed practical nurse, said in a witness statement that she wanted to send Maria “out right away but the son refused for resident to be sent out even though I told him that resident is in (sic) severe pain and is unable to stand.”
In the statement, written shortly after the incident took place, Cromwell said Larry wanted the X-ray to be done on December 26 and “stated that at this point he does not know if anything can be done.” Larry disputes this characterization.
Cromwell also wrote she asked another employee Kiana Waters to observe the phone call as a witness. Waters, in a statement taken Jan. 6, 2022, wrote that she was sitting at a desk when she witnessed the fall. She wrote she could not get up quickly enough to grab Maria from falling.
Waters also described Larry as hesitant to send his mother to the hospital.
Records show that Maria received an X-ray exam on Christmas at Arden Courts. It confirmed a fractured right hip. The radiology report was signed by a physician just after 8 p.m.
The Talleyville Fire Company then arrived within the hour for Maria. In a report, paramedics said they found Maria in bed, “screaming in pain at the top of her lungs.” The 86-year-old was in “obvious distress and severe pain.” They found that her leg was rotated, swollen in the hip area and “severely tender.”
Staff told the paramedics that the patient fell a “few hours ago” and they called a mobile X-ray company to perform the test. They waited for the results before calling 911, according to the report. Arden Courts did not respond to The News Journal’s questions on why an X-ray was conducted several hours after Maria fell.
“The nurse did not give a full report and did not know any history on the patient,” the report reads. “The nurse also would not see how the patient fell or what happened. The patient was moved from where she fell back into her bed with the severe pain she was in.
“When staff was (sic) questioned about this they had no answer.”
Danny was the first to arrive at the hospital. He recalled his mother saying a “son-of-a-(expletive)” pushed her. Her stubborn feistiness, in such a distressing moment, made him laugh. It was the last full conversation the two shared.
Arden Courts Executive Director Tina Larose, in a conference call following the incident, Larry recalled, told him the person who pushed Maria was a man who had no history of previous violence.
INSIDE LEG HALL: Why no one seems to agree on how to improve dementia care inside Delaware long-term care
In emails reviewed by The News Journal, Larry wrote to Larose repeatedly asking the facility for more information on how this happened. The facility declined to directly give the Rufos the incident report, citing privacy concerns, and said video footage did not exist.
“We need this not only for our own peace of mind but to help understand how she was injured,” Larry wrote in a Dec. 30 email. “The doctors at the hospital keep asking us and we quite unbelievably have to tell them we do not know.”
A health department spokesman said Arden Courts was required to submit a 5-day follow-up report to DHCQ following Maria being pushed. This type of report is “the facility’s internal investigation and includes the root cause of the incident, the outcome of the investigation, any care plan and/or system changes that were implemented as a result,” according to the spokesman.
Based on the follow-up report, the spokesman said, a licensure survey was not conducted. But DHCQ’s investigative unit did look into the incident, confirming that abuse occurred.
The incident report noted that Maria was pushed in the hallway, with her injuries being defined as “serious.” The resident who pushed Maria, according to the document, was “not aggressive with staff.” He was placed on 30-minute checks.
There was no information listed detailing any care plan or system changes.
Later, with the onset of litigation in 2023, the family learned in an Arden Courts employee’s witness statement that the man “put his hand out and grabbed her by her neck and he pushed her.”
Maria was discharged from the hospital on Jan. 11, 2022, to the nursing home now called ProMedica Skilled Nursing and Rehabilitation, located just yards from Arden Courts. When Larry and Danny visited her for the first time, they could hear her scream as they walked down the hallway.
She was in bed in a room by herself. She repeatedly cried out for her mother in Italian.
Days later, Danny returned to the nursing home alone. Maria had entered hospice by this point. He noticed her fingernails hadn’t been cut lately, so he brought a small nail clipper with him. It was something he always used to do for her.
He talked to her, even though she couldn’t talk back. He said goodbye.
Maria died hours later.
The Rufo brothers buried their mother at the cemetery, in a tomb with their father. It’s where their grandparents and other family members are also buried. As a boy, Maria’s mother would tell Danny that one day, he would visit them all in the cemetery.
“I drive by that cemetery on Lancaster Avenue,” Danny said, “and I look straight ahead sometimes.
“I’m still dealing with it.”
Does your family have an experience with a Delaware assisted living facility? Fill out this form. To contact reporter, Meredith Newman, email her at mnewman@delawareonline.com or call her at 302-256-2466.
This article originally appeared on Delaware News Journal: Dementia care facilities in Delaware go uninspected

