Understanding COVID-19 antibody tests
- Oops!Something went wrong.Please try again later.
Adam’s Journal
Here’s a question from a reader:
My husband and I were fully vaccinated against COVID-19 in January 2021, and we received booster doses in October. I received Pfizer shots, and my husband got Moderna. Last month, blood tests showed we were negative for COVID-19 antibodies. Why would that be?
— Cathy Arthur, Oklahoma City
Dr. McEver Prescribes
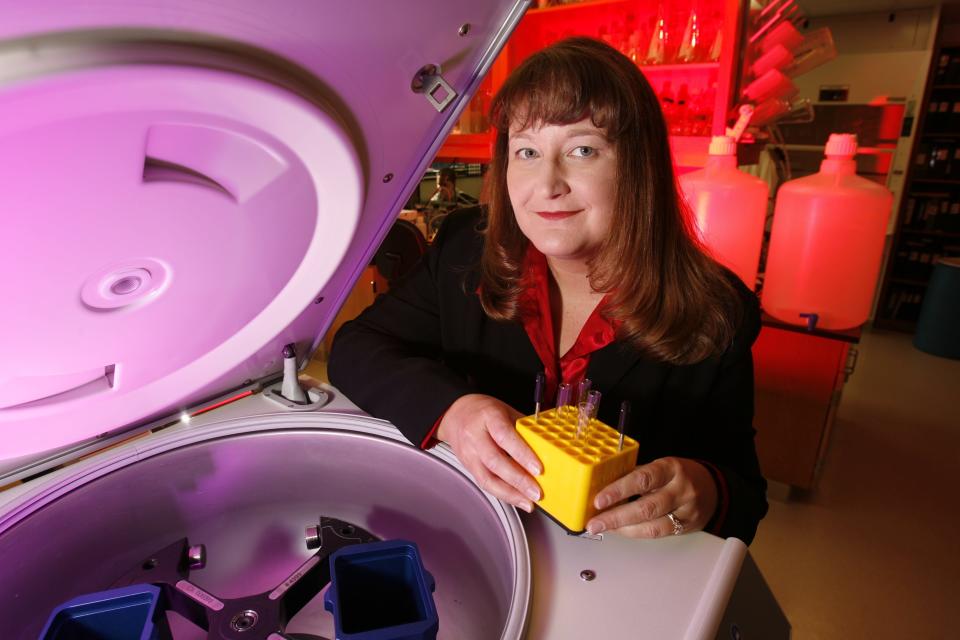
For this question, I consulted Judith James, M.D., Ph.D., who leads the Oklahoma Medical Research Foundation’s studies of the body’s immune response to COVID-19. James is an immunologist, board-certified rheumatologist, and OMRF’s vice president of clinical affairs. Here’s what she said:
Not all COVID-19 antibody tests are created equal. The most likely reason your tests yielded negative results is because of what they were measuring.
Early in the pandemic, scientists developed antibody tests to confirm whether a person had previously been infected with SARS-CoV-2, the virus that causes COVID-19. These blood tests look for an antibody against a particular COVID protein called the nucleocapsid. This protein is found inside the virus and is only present in those who have survived infection.
The vaccines approved for use in the U.S. include only a piece of the virus, the SARS-CoV-2 spike protein, found on the surface of the virus. Antibody tests measuring responses against the nucleocapsid protein don’t detect antibodies against the spike protein. Therefore, if you had a test that measures nucleocapsid antibodies, you could be negative — meaning you haven’t been infected but could still have antibodies against the spike protein from vaccination.
Tests that detect anti-spike antibodies are available, and you could specifically ask for this test. Even if you can’t make anti-spike antibodies for some reason, your immune system also has other components — like T and B cells — that often can contribute to long-term defenses.
An extremely small fraction of vaccinated individuals may not make a strong antibody response.
Usually, these people either have impaired immune responses from diseases, like the autoimmune diseases we study at OMRF, or are on medications to suppress their immune system from cancer, autoimmunity or for transplantation. OMRF is helping lead a nationwide National Institutes of Health-funded study to find ways to improve the responses in these patients.
Your antibody test results shouldn’t be cause for concern. With three doses of vaccine, you and your husband have dramatically decreased your risk of developing severe COVID-19. However, with the number of cases we are currently seeing in our communities, masking and social distancing are still important additional protective steps.
McEver, a physician-scientist, is vice president of research at the Oklahoma Medical Research Foundation. Cohen is a marathoner and OMRF’s senior vice president and general counsel. Submit your health questions for them to contact@omrf.org.
This article originally appeared on Oklahoman: Bodywork: Understanding COVID-19 antibody tests
