A visit with your doctor is not what it used to be. What to know about telemedicine
Five-year-old Toyam Marathe FaceTimes his grandmother once a week. He touches his school photo every day, a sign his mom says means he’s missing school, even though his class is on Zoom now.
He also has two weekly virtual therapy sessions with Julie Cristello, a doctoral student from FIU’s Center for Children and Families.
He’s adapted fairly well to the situation, a relief for his mother, Nicole Jackson, who was worried about his routine being disrupted. Toyam was diagnosed with selective mutism, or SM, an anxiety disorder. Children who are diagnosed with SM are usually talkative at home but are unable to speak in other social settings such as school.
The Broward County mom says she never liked the idea of using a telehealth service for her son’s treatment. She always thought face-to-face sessions were better. It’s one of the many reasons why she started driving Toyam in September 2019 to FIU’s main campus on Southwest Eighth Street for weekly sessions at the FIU center’s clinic.
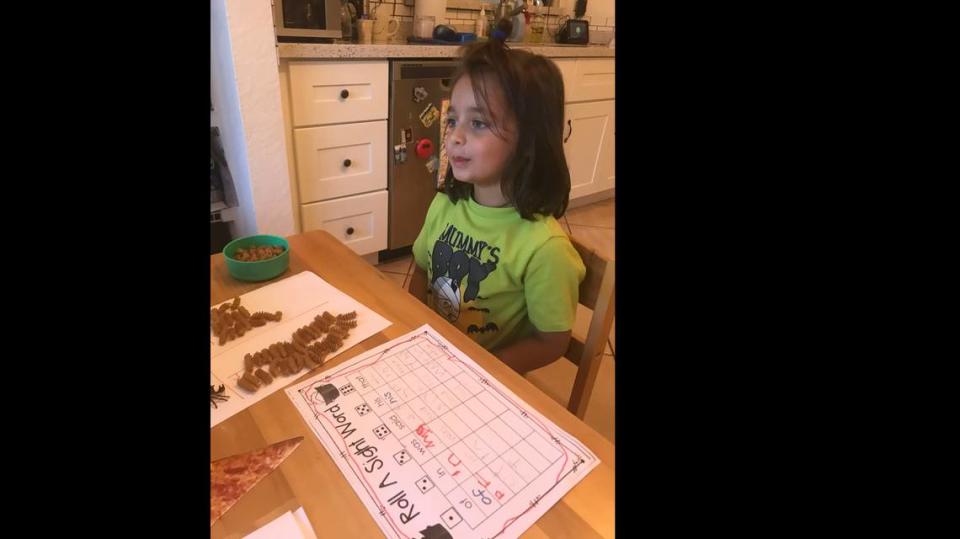
From her Deerfield Beach home, the trip can take up to an hour and half to arrive. Its worth it for Jackson who has seen improvements with Toyam since he began the sessions. But then COVID-19, the disease caused by the novel coronavirus, began spreading across the world.
Businesses began closing, schools went online and restaurants converted into takeout and delivery only to limit the spread of the disease in Florida. The shutdown also made Stage Kitchen and Bar in Palm Beach Gardens, a restaurant Jackson and her husband opened in February, convert into a takeout spot.
Then FIU’s center called — they were transitioning services online. Was she still interested?
Worried that her son’s progress would stall or regress, Jackson agreed to try it. Six virtual sessions later, including one that involved Cristello, Toyam and his teacher Kristin Hill of Summit Questa Montessori, her opinion on virtual sessions changed. Now, she wishes she would have moved his sessions online sooner.
The online sessions are convenient, and her son is still engaged and seems to enjoy them, she said. Now, she’s thinking of doing a mixture of face-to-face and virtual sessions, if the option is available, once life goes back to normal.
But like most first time telehealth users, Jackson had a variety of questions, including how effective treatment would be.
Here are answers to some of the most common questions people might have about using a telehealth service:
What is telemedicine, how does it work and who offers it?

Telemedicine lets health professionals — including doctors, dermatologists and therapists — evaluate, diagnose and treat patients remotely. Visitations can be done by phone or live video (typically through a HIPAA-compliant secure video platform). Medications can still be prescribed during a virtual visitation.
That means you can stay home, watch the kids and not worry about social distancing. While telehealth has been around for several years, more and more people are requesting virtual visitations during the COVID-19 pandemic.
Telehealth usage increased by 50 percent nationwide in March, with telemedicine providers such as Teladoc reporting a spike in video requests to more than 15,000 per day, according to CNBC. Analysts told CNBC they are expecting “virtual healthcare interactions” to top one billion by the end of this year.
Doctors and other healthcare providers are using virtual visits to treat COVID-19 symptoms and other non-emergency medical needs. Here are some of the places offering virtual visits or services in South Florida:
Baptist Health of South Florida is offering free 24-hour online urgent care visits through its Care On Demand app for anyone who is experiencing symptoms similar to those of COVID-19. Symptoms include fever, coughing and shortness of breath. For the free virtual visit, use the code “Care19.”
Bowes Dermatology by Riverchase is offering virtual visits to diagnose and treat different skin conditions through video chat. During the consultation, screenshots may be taken of your lesion or you may be asked to send pictures for further evaluation following the virtual visit. To learn more about the process or to request an appointment, visit https://www.riverchasedermatology.com/virtual-visits/.
Jackson Health System in Miami is offering telehealth appointments to continue preventive care and medical attention remotely to its patients. To request an appointment, call 305-585-4564.
Memorial Healthcare System in South Broward offers telehealth services to treat non-emergency, minor medical concerns including asthma, sinus infections, strep throat and the flu. Its also offering free virtual doctor visits for COVID-19 inquiries. Use the code “MEMORIALCARES.”
University of Miami Healthcare System offers virtual visits for more than a dozen specialties including arthritis, cancer, diabetes, primary care, sleep medicine, dermatology and ear, nose and throat. To learn more about the different virtual clinics, visit https://umiamihealth.org/en/Treatments-Services/virtual-clinics.
UHealth’s 24-hour MyCareConnection, which typically treats symptoms such as nausea, the flu, headaches and respiratory problems also is offering COVID-19-related consultations by phone or video chat. Virtual visits are $59 or less. To make an appointment through MyCareConnection, visit https://umiamihealth.org/treatments-services/telehealth-virtual-visits
Broward Health offers 24-hour access to physicians who can determine if you need to be tested for COVID-19 and give advice depending on whether they consider you to be a no-risk or high-risk patient through its BHealthy Now app. You can get a free screening by entering the code “BHealthy.”
To find the app, you will have to search for “Amwell” in the app store and then enter the Service Key “Broward” during or after enrollment for the Broward Health COVID-19 practice.
Does my insurance cover telemedicine? Are virtual visits available 24/7?

It varies by insurance and service so you’ll always want to inquire with your insurance company or check your policy first. Double-check with the doctor’s office too to make sure they offer the service you’re requesting and that they accept your insurance.
While some insurances already included telemedicine coverage, others have added or expanded coverage because of the COVID-19 crisis. Here are some examples of what you can expect:
Aetna is offering a $0 copay for phone or video chat telemedicine services until June 4. The insurance says its waiving costs for all telemedicine visits through network providers who deliver virtual care, Teladoc options available through the Aetna Health app and through other virtual care apps or services provided as part of your plan.
Blue Cross Blue Shield (BCBS) expanded coverage for telehealth services at all 36 locally based, independently operated BCBS companies and the BCBS Federal Employee Program. Collectively, the BCBS system is also waiving telehealth copays and cost-sharing for telehealth services, with some health plans offering additional telehealth resources by region.
Cigna is waiving customer cost-sharing for telehealth screenings for COVID-19 through May 31. It’s also providing free home delivery of up to 90-day supplies for Rx maintenance medications available through the Express Scripts Pharmacy, 24/7 access to pharmacists and has created a free interactive COVID-19 risk assessment tool. The insurance company also has a database that can help connect you with a doctor or nurse virtually 24/7.
Medicare has temporarily expanded its coverage of telemedicine services to give patients access to virtual visits from a range of providers such as doctors, nurses, practitioners, clinical psychologists and licensed clinical social workers. The expanded coverage gives patients the ability to request virtual visits from more places (including homes) by using a “wider range of communication tools” such as smartphones.
During the pandemic, patients will be able to receive evaluation and common office visits, mental health counseling and preventive health screenings without a copayment if you have Original Medicare. The federal insurance will also pay for “virtual check-ins.”
United Healthcare is waiving member cost-sharing for the treatment of COVID-19 until May 31 for Medicare Advantage, Medicaid, Individual and Group Market fully insured health plans and has a database of doctors and nurses available for virtual visits 24-7.
Its also offering a free 24/7 emotional support line staffed by professionally trained mental health experts. The hotline 866-342-6892 is free and open to anyone. The company also has a free on-demand emotional support mobile app called Sanvello with resources to help you cope with stress, anxiety and depression during the COVID-19 pandemic.
Are telemedicine services available for mental health?
Dr. Jonathan Comer, a psychology professor at Florida International University, says telehealth has “played an important role” in the mental health field for years. He says the current COVID-19 crisis and social distancing regulations has pushed the majority of mental health providers, if not all of them, to temporarily move their services online, with exceptions for “acute crises.”
And virtual sessions are just as effective as face-to-face sessions, he said.
Comer is the director of FIU’s Mental Health Interventions and Technology (MINT) Program, which offers a range of in-office and telehealth mental health services for children under 18. His clinic has found through more than a decade of research that when it comes to certain types of treatments, such as those for child anxiety and parent coaching for behavioral problems, live virtual sessions help “overcome accessibility of care issues” and gives the clinician the ability to treat the families in their natural environment.
“Technology can even improve upon the effectiveness of care by intervening directly in the settings that are most problematic,” Comer said.
The nature of child anxiety calls also appear to be changing during the COVID-19 shutdown, he said. The program’s anxiety clinic normally receives calls about separation and social anxiety, he said, but now there’s an increase of calls relating to COVID-19, germs, contamination and infection.
He said the clinic is also receiving more family conflicted-related calls because of the stay-at-home orders, including stressed parents who are working and having to home school their child.
How safe is my privacy during virtual visits?

While Facebook Live, Twitch, TikTok and other “public facing” platforms are still prohibited for telehealth services, technology regulations have relaxed during the COVID-19 pandemic to allow doctors to use apps like FaceTime, Facebook Messenger, Google Hangouts, Zoom, or Skype to vidoe-chat with their patients, according to the U.S. Department of Health & Human Services.
But HIPAA still applies for virtual visits which means you are still entitled to confidentiality, said Dr. Erika Coles, the clinic director at the FIU Center for Children and Families which offers a wide-range of mental health programs for kids, including anxiety and depression.
Some telehealth providers will explain the virtual security measures on a webpage dedicated to the service, but if you have any questions about the service, contact them and ask.
In the center’s case, Coles says they are using a HIPPA-compliant version of Zoom, which has more privacy protections, to conduct their live video chats with clients and are also offering services through the phone for patients who don’t have access to a reliable Internet or don’t have a device with a webcam feature.
Families received a telehealth consent form explaining the policies and procedures, and the staff members were trained on some of the challenges they might face while working from home to ensure the client confidentiality privilege is not broken, she said.
“We’re protecting the privacy of our clients,” she said, “by making sure we don’t have other members of our family being able to overhear the session, making sure that we’re not recording anything about the client session ... having a private WIFI and making sure we’re not using a public WIFI — all these things that kind of come up in particular with telehealth.”
To learn more about the center’s services, visit https://ccf.fiu.edu/

