Why it's time to stop living in fear of COVID
- Oops!Something went wrong.Please try again later.
- Oops!Something went wrong.Please try again later.
The balance of power between human and virus is shifting. Better armed against a lesser enemy, our species no longer needs to hide in a bunker waiting for a viral wave to pass. That means it’s time for our COVID-19 response to change.
As we enter the “endemic” stage of the virus, however, there is confusion about what an updated approach should look like.
On Monday, Spanish Prime Minister Pedro Sanchez called for a Europe-wide discussion about developing the kind of response that exists for, say, the flu. The U.K. has extended its “Plan B” rules for another three weeks, but has softened its testing and travel policies and Prime Minister Boris Johnson is under pressure to lift existing restrictions.
It’s too early to declare victory. Infections are rising sharply, and there are still a worrying number of deaths from COVID-19. Plus, there are many regions where health services are under extreme pressure.
And yet, the overall pandemic picture gives cause for optimism. Omicron infections in South Africa peaked about a month after the wave began. And data from multiple countries show the latest variant, while far more transmissible, is causing less severe disease — with lower levels of hospitalization, shorter hospital stays and fewer deaths.
One explanation is that omicron appears to affect the body differently than previous variants. A study from the University of Hong Kong Faculty of Medicine suggests omicron may replicate in the lung more slowly than delta, which would give the immune system more time to respond.
Natural immunity also accounts for a lot. In countries where infection rates were relatively high in earlier waves, susceptibility to serious illness with omicron seems much lower. A study published Monday by London’s Imperial College confirms that even immunity from the coronaviruses that cause the common cold may help bolster defenses against SARS-CoV-2.
Most importantly, though, vaccines (and especially booster shots) have led to dramatically lower levels of hospitalization and death. Indeed, the unvaccinated account for the large majority of serious COVID-19 hospital cases everywhere.
What restrictions do we need as we move into the endemic era? Let’s first look at what we can do away with. Self-isolation requirements, for one. The Centers for Disease Control and Prevention in the U.S. reduced self-isolation from 10 days after a positive test to five days. The U.K. has now amended its own rules to allow people to stop self-isolating earlier if they get two consecutive negative lateral flow tests on days six and seven.
The old self-isolation rules make little sense for a virus that has the severity of the common cold in most cases. It is an enormously costly policy, especially when you consider the teachers and health-care workers who must stay home after a positive test, even when they have no symptoms and could work safely with masks.
Government guidance in places where vaccination rates and natural immunity are high should be simple: Anyone with symptoms remain at home while unwell. It is also prudent for people to wear masks on public transport and in crowded public spaces, during peak flu/cold seasons, and if they have been unwell. Making high-quality masks, such as N95 or FFP3s, freely available may help encourage their use.
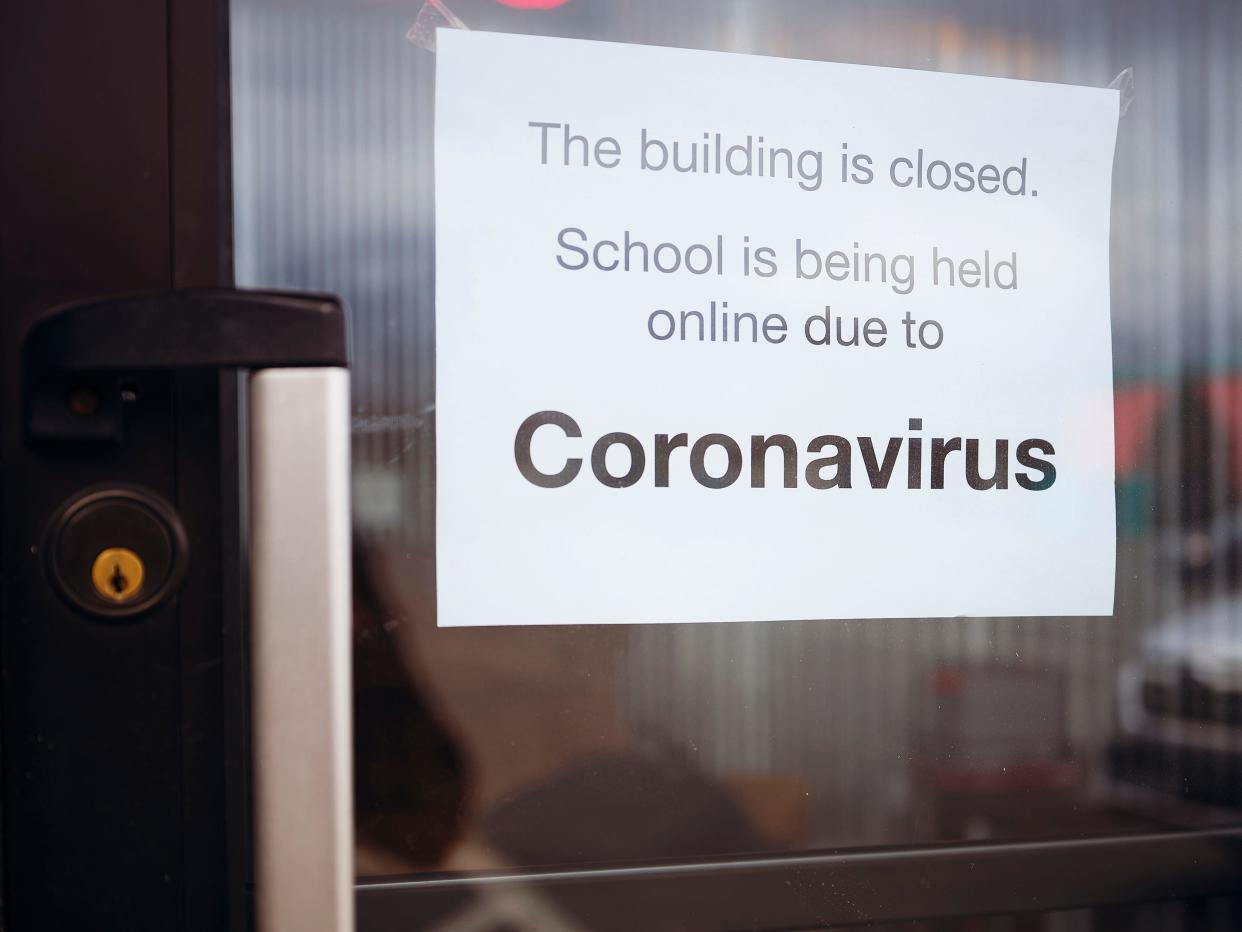
Work-from-home rules and schooling also need rethinking. Remote learning carries enormous social, mental health and economic costs.
Finally, we’ll need to consider how much vaccinating to do beyond a third dose. With a virus of waning severity and rising levels of natural defenses, it’s not clear we need an entire population to be routinely re-vaccinated after the third shot if the variants in circulation remain mild. It may be enough to offer variant-specific vaccines to over-60s and other vulnerable groups every six or 12 months, while making further vaccination optional for others.
Obviously, public health measures need to be under constant review. We must also continue to monitor levels of immunity and to test and sequence rigorously. Endemic doesn’t mean harmless. Malaria and tuberculosis are also endemic in some parts of the world — and there were 627,000 malaria deaths and 1.5 million tuberculosis deaths in 2020. Long COVID — a complex illness where infected people suffer debilitating symptoms for months or longer — is another reason not to get complacent.
Scientists have pointed out there is nothing to prevent a more battle-hardened SARS-CoV-2 variant emerging again. But that risk doesn’t justify long periods of costly restrictions right now. Levels of vaccination and immunity, and access to hospitals and treatment, should determine levels of restriction — not infections. Endemics demand different responses, as do milder diseases. This isn’t a return to the false dichotomy of lives versus livelihoods from earlier waves; the virus has changed, as have our defenses.
At the moment, the bark of SARS-CoV-2 looks worse than its bite. We’d be wise to adjust accordingly.
Therese Raphael is a columnist for Bloomberg Opinion and former editorial page editor of the Wall Street Journal Europe. Sam Fazeli is senior pharmaceuticals analyst for Bloomberg Intelligence and director of research for EMEA.
This article originally appeared on Palm Springs Desert Sun: Why it's time to stop living in fear of COVID

