This Woman’s Toothache Medication Actually Turned Her Blood Blue
A 25-year-old woman started turning blue after using “large amounts” of topical benzocaine (a numbing agent) for her toothache, a new case report in The New England Journal of Medicine finds.
The woman was diagnosed with a blood disorder called methemoglobinemia.
A toxicologist explains how methemoglobinemia forms, what causes it, and the potential risks associated with the condition.
When you take medication, you expect that it will work to make you feel better. What you don’t expect is that it will turn you blue. Unfortunately, that’s what happened to one woman in Rhode Island—and she ended up in a case report.
The 25-year-old woman, who was not publicly identified, went to an emergency room in Providence, Rhode Island, with generalized weakness, fatigue, shortness of breath, according to The New England Journal of Medicine. She was also concerned about the fact that she was, you know, turning blue.
After evaluating her, the woman’s doctors determined that she was turning blue thanks to a numbing agent she had used. “She reported having used large amounts of topical benzocaine the night before for a toothache,” the case report authors wrote.
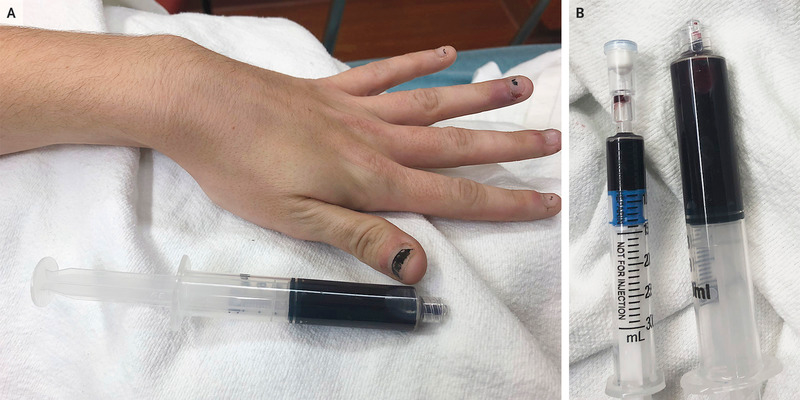
The woman was diagnosed with methemoglobinemia, a blood disorder where an abnormal amount of methemoglobin is produced. Methemoglobin is a form of hemoglobin, the protein in red blood cells that carries and distributes oxygen to the body, according to the U.S. National Library of Medicine. However, it is a dark pigment that causes blood to appear very dark in color, says Jamie Alan, PhD, an assistant professor of pharmacology and toxicology at Michigan State University.
“There is normally a small percentage of this compound in the red blood cells, however it is kept very low,” she explains. “But certain compounds like benzocaine can accelerate the formation of methemoglobin.” The result? Hemoglobin cannot successfully release critical oxygen to the tissues, so the body turns blue.
How do people get methemoglobinemia?
Methemoglobinemia is usually either inherited from your family or caused by exposure to certain chemicals, medicines, or foods, the U.S. National Library of Medicine says. Those can include anesthetics like benzocaine, nitrobenzene (which is used in some drugs, pesticides, and dyes), certain antibiotics like dapsone and chloroquine, and nitrates (which are used as additives to keep meat from spoiling).
Benzocaine “and similar compounds used to be in infant and children’s teething gels, but it was taken out of those products because of this exact thing,” Alan says.
What are the symptoms of methemoglobinemia and how is it treated?
A bluish tint to the skin is a major symptom of methemoglobinemia, but a person can also have a headache, giddiness, altered mental state, fatigue, shortness of breath, and lack of energy.
Methemoglobinemia is “very harmful,” Alan says. “The problem is that methemoglobinemia reduces the ability of your red blood cells to carry oxygen. This can lead to heart attack, stroke, organ damage, and death,” she adds.
A medication called methylene blue is used to treat severe cases of methemoglobinemia and ascorbic acid (aka vitamin C) can also be used to reduce the amount of methemoglobin in a patient’s blood, the U.S. National Library of Medicine says. Undergoing hyperbaric oxygen therapy, a blood cell transfusion, and exchange transfusions (where a person’s blood is removed and replaced) can also be helpful.
People don’t usually need treatment for mild cases of methemoglobinemia, though—they should just avoid the medication or chemical that caused their condition in the first place. “The half life of methemoglobin is 55 minutes, meaning the condition will usually reverse in hours,” Alan says. “In the meantime, the patient needs supportive care with oxygen.”
If you suspect you’ve developed methemoglobinemia, see a doctor immediately.
Like what you just read? You’ll love our magazine! Go here to subscribe. Don’t miss a thing by downloading Apple News here and following Prevention. Oh, and we’re on Instagram too.
You Might Also Like

