'A world that doesn’t understand': New Hampshire's veterans share how they asked for help
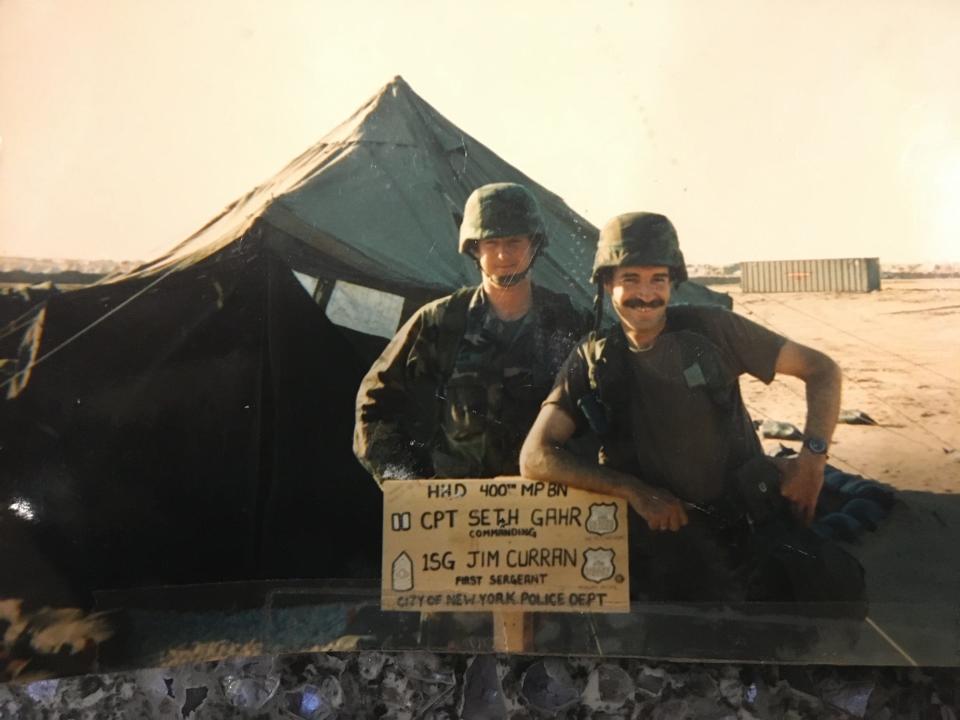
Seth Gahr of Stratham is a New Hampshire State Police trooper and retired Army lieutenant colonel who served in Iraq during both Operation Desert Storm in 1991 and the Iraq War following the terrorist attacks of Sept. 11, 2001. He was also a New York City police officer and first responder to the World Trade Center on 9/11.
Today, as the coordinator of the New Hampshire State Police Peer Support Unit, he’s working every day to get military veterans and first responders the mental health care they need and the benefits they have earned.
Service members rely on each other during war, and veterans trust and understand each other. Many who serve together remain close for the rest of their lives. So, when a New Hampshire veteran is in crisis, it is very often Gahr who is dispatched to help.
“The hardest part of any war is not the war itself, but coming back from the war,” Gahr said.
This is the seventh story in a year-long collaboration on mental health between Seacoast Media Group, New Hampshire Union Leader and Dartmouth Health. https://www.seacoastonline.com/in-depth/news/2022/11/27/nh-veterans-mental-health-struggles-suicides-resources-va-support/69655342007/
Kevin O’Brien, of Merrimack, who retired as a staff sergeant in the Air Force, described the feelings of isolation transitioning from active duty to veteran status.
“You put on that uniform, and you almost feel like Superman," he said. "You get this overwhelming sense that 'I’m doing what a lot of people will never do.' And then you come back from overseas and you’re just getting out of the military and you’re coming back to a world that doesn’t understand you. They don’t want to understand you. Some people are afraid of you. And we’re afraid to talk about what we’ve been through because no one is going to understand.”

O’Brien's goal was a career in law enforcement, and he was well on his way working in military security forces at Lackland Air Force Base in Texas. While deployed, he blew out two discs in his back doing demolition work on a base in Pakistan. Several unsuccessful surgeries later, he was retired from the military, disabled and his hopes of a career in law enforcement were gone forever. As his career ended, his marriage fell apart and he lost visitation rights to see his son.
“So that pressure, on top of my surgeries, on top of my career, I’ve just lost my whole family, too,” O’Brien said. “I don’t get hooked up with the VA (Veterans Affairs) until 2012. And then I go through doctor after doctor after doctor, pill after pill after pill.”
After a suicide attempt in 2013, he said, he wound up in the VA hospital in Brockton, Massachusetts, a facility with conditions so poor at the time they made national headlines.
“My time with the VA has been quite strained,” O’Brien said in an email he sent following an interview for this story. “While I am lucky now to have a solid team, that was not always the case. When I got out, I was only considered 30% disabled due to my spinal fusion. I was never prepped properly for separation/retirement. The past 10-11 years have been a battle for me to get the 100% disabled I am today. I have had to prove time and time again that my injuries are legitimate and should be attended to properly. It’s not an easy system, especially when you’re brand new and have no one to direct you properly.”
Veteran suicides a cause for alarm
While mental illness touches as many as one in four Americans, it hits our nation’s veterans harder. Veteran rates of suicide, substance misuse, depression and anxiety are significantly higher than the rates for non-veterans.
“In 2020, adjusting for population, age and sex differences, the suicide rate for veterans was 57.3% greater than for non-veteran U.S adults,” the VA reported in 2022. “In 2020, there were 6,146 veteran suicides. This was an average of 16.8 per day.”
New Hampshire’s veteran suicide rate in 2020, 36 per 100,000 is “significantly higher” than the national veteran suicide rate of 31.7, according to the VA.
In 2021, there were 87,604 veterans in New Hampshire, or 7.8% of the population aged 18 and over, according to the U.S. Census Bureau.
Who are our veterans in the United States? We examine the population of those who served. https://www.usatoday.com/in-depth/graphics/2022/11/11/veterans-day-five-charts-profile-status-of-veterans/8292080001/
While not all suicides are mental health-related and not all veterans struggling with mental health challenges become suicidal, they are an indicator that veterans and their families are struggling, said Susan Stearns, executive director of NAMI-NH (National Alliance on Mental Illness-NH).
“Suicide is a huge indicator of the bigger picture,” Stearns said. “It really is about what kind of supports and care do our veterans need.”
Barbara Van Dahlen, a nationally renowned clinical psychologist, co-chaired former President Donald Trump’s PREVENTS program, an acronym for “Presidents Roadmap to Empower Veterans and End a National Tragedy of Suicide.” After deep study, she noted: “Suicide is an indicator of the impact of stress. We know that veterans are at a higher risk for suicide. Period. It is a risk factor.”
Dr. Brett Rusch, a psychiatrist and executive director of the VA Hospital in White River Junction, Vermont, said mental illness and suicidal ideation most often build up over time.
“Rarely have I spoken to a veteran who says, ‘Oh, here is the one thing that happened that changed everything,’” Rusch said. “More commonly what I hear is a series of stories that have built upon each other, creating more burden over time.”
What is causing the high rates of veteran mental illness and suicide?
There are many reasons veterans suffer mental illness at higher rates than non-veterans. Some are related to the demands and trauma of military service, whether in combat or support roles. But military culture and bureaucratic barriers to receiving help also play a role.
There are dozens of organizations committed to helping New Hampshire’s veterans receive the care they need, from the large VA hospitals in Manchester and White River Junction to newer nonprofits like Hero Pups in Stratham, which matches veterans with service dogs. All those interviewed for this story point to recent improvements in the treatment and care of veterans, but also acknowledge the state and nation have a long way to go in the treatment and care of men and women who served.
“There is help and there is hope,” said O’Brien, who now shares his story through NAMI-NH. “Don’t give up. There is someone out there to talk to. It may be another vet, or a husband or a wife. Someone would rather listen to you for six and a half hours than carry you to the grave.”
Help is available, but not always easy to access.
“There’s no easy way for veterans to go to the computer and Google ‘Help For Veterans’,” Van Dahlen said. “They’ll get inundated with stuff. And so how do you know what’s good, what’s not?”
Dr. Rusch said any veteran who contacts the VA will receive mental health care and guidance on the same day they reach out for help.

“If you just walked in, whether it is to the primary care clinic, to the emergency room or really, frankly to any desk in our hospital and said. ‘Hi, I’m a veteran, I’ve never been here before,’ we would navigate you through the system to the point that you’d be able to have (contact) with a mental health counselor or professional of some kind before you left.”
He also urged everyone to know and use the veterans crisis line, 988, which went into full effect in July. Call 988 and press 1 and you will be connected to a veteran service officer who can help. He encouraged those who love and support veterans to have that number in their phone contacts.
“You never know when you’re going to be in a situation to help somebody,” Rusch said.
Kevin Forrest, an Army veteran who is the director of the Manchester VA, said that veterans in crisis will always receive immediate attention.
“We have same-day access for veterans that are in crisis or feel they need to be seen for any reason for mental health,” Forrest said.
Because Manchester does not have inpatient mental health beds, if a veteran needs inpatient or a higher level of care, Manchester will connect them with full-service VA hospitals in White River Junction, Boston or beyond.
“We work with those programs to get a bed and then transport the veteran to those locations,” Forrest said. “We have not had to turn a veteran away who needed an inpatient bed and we have not had to board people. It doesn’t always mean we can get folks into the closest place that we’d like to get them in, but we are able to get them in for care.”
Roughly 27,000 veterans are enrolled at the Manchester VA and another 10,000 at White River Junction, Forrest said.
No wrong door for veterans to get help
Jamie Cummings, a veteran service officer at the New Hampshire Office of Veterans Services, said her division has a “no wrong door” policy, meaning that even if they are not the people who can help directly, they will find the people who can and make a warm handoff.
Cummings spoke very highly of the state’s vet centers, which are part of VA but smaller and, some clients tell her, less intimidating places to begin their mental health care journey.

“A lot of clients will feel more comfortable engaging with the vet center first and then going to a VA medical center or outpatient clinic to get in touch with a psychiatrist,” Cummings said. “I look at it like a bridge where they can get good solid counseling and they have veterans on staff that are counselors there who may make someone feel comfortable about going to see a psychiatrist about medications.”
Dr. Rusch said the vet centers are “run by people who are themselves veterans and so they bring a certain perspective to mental health treatment that comes from a place of lived experiences.”
Trooper Gahr, who works closely with Cummings, encouraged veterans to reach out for help.
“The vets don’t need to be shy,” Gahr said. “They can just walk into a VA and say, 'I’m a veteran and I have a problem' and they’ll be taken care of at the door. The vet centers and the VA, they’ll take care of you.”
Cummings said VA care has come a long way since the Vietnam era.
“This is not the same VA of the 1970s,” Cummings said. “Not even close.”
Risk factors for veterans start during military service
Barbara Van Dahlen said that mental health stressors begin almost immediately upon enlistment.
“The journey begins when you sign on the dotted line and raise your hand and say, 'I will serve my country,'” Van Dahlen said. “But the experience of being in the service and the challenges and the risks, they contribute to the risk factors for our veterans.”
Van Dahlen said many young men and women who join the military are leaving home and family for the first time.

“There are pretty intense demands on them physically and emotionally,” Van Dahlen said. “Some wash out during those initial training weeks, but those who go on, the pressure builds.”
Unlike civilian life, she described the military as “a quasi-family situation where you have people telling you what to do about everything.” On top of this, service members and their families are constantly moving, so there is limited connection with a non-military community. Further, they are not managing personal finances as they might need to outside the military.
“You have these young families trying to make it on a relatively limited budget,” Van Dahlen said. “It’s very difficult for military spouses to get jobs. So there’s tremendous financial stress and sometimes they get themselves into trouble because they don’t always know how to manage that.”
Those leaving the service often have difficulty explaining their highly skilled military work to civilian employers.
“Someone comes out of the military, they want a job, they go speak to some company and their job skills don’t translate,” Van Dahlen said. “We saw this a lot during the war years. These men and women who were literally considered heroes because of what they put themselves through and how they served would come out and they couldn’t get a job that made them feel respected or valued.”
Substance misuse is a major problem.
“Perhaps as many as one in four and maybe more struggle with addiction, whether it’s to prescription pills or to alcohol or other substances” said Dr. Rusch said. “And that’s before you even get to vulnerabilities for post traumatic stress disorder, for depression, for anxiety and other circumstances.”
Sexual assault in the military is an issue gaining greater attention and the PACT Act just signed into law attempts to address the damage done by toxic burn pits, agent orange and other chemical exposures.
Military culture focused on combat, not counseling
One less-discussed health risk factor, however, is the military culture itself, which veterans understand to mean that mission goes above self and that commitment to country and your brothers and sisters in arms is more important than any physical or mental ailment you might suffer.
“In the military, we gut it out,” said Gahr. “Everybody guts it out. You can’t go to a medic if something bothers you. Because you’re a warrior. You have to fight. You don’t have time to say, ‘It’s time out, I injured myself.’ Everybody is hopped up on adrenaline. Nobody wants to go see the medic, to come off the line. ... Years later, it starts to hurt. Years later, these injuries start popping up.”
O’Brien said he didn’t seek help until the pain became unbearable because he thought it would take him away from the mission.
“They tell you that mental health support is there to help you," O'Brien said. "I carried a gun. Do you think I want to go to mental health so they can take my gun away and so they can take my job away so I can sit at a desk. That’s not why I signed up. I’ve signed up to do a job that no one else will do. And if I have to suck it up and deal with my own then I’m going to suck it up and deal with my own.”
Dr. Rusch said most in the military are “driven to serve.”
“It’s the attitude toward injury that it is something to be seen as only a temporary inconvenience,” Rusch said. “A lot of them will sustain multiple injuries that bring not only physical consequences but psychological consequences as well. I’ve heard stories of tremendous psychological trauma both witnessed and committed in pursuit of mission.”
The difficult transition from service member to veteran
The first year of transition from active duty to veteran is fraught with risk. To address this, VA and other federal agencies offer a specially designed Transition Assistance Program (TAP) to help service members moving from military to civilian life.
But there are roadblocks.
First, the Department of Defense’s CERNER electronic health records system is not linked to the VA medical records system so each service member comes to the VA as a blank page. Often, at the end of service, members are eager to get home, not focused on collecting documentation of physical or mental injuries. Accessing medical records is a challenge that often requires help from someone like Jamie Cummings at the New Hampshire Division of Veterans Services.
Help support quality local journalism like this. Subscribe today.https://subscribe.seacoastonline.com/offers
Dr. Alicia Semiatin, the chief of mental health services at the Manchester VA, said the "Military to VA" program is focused on addressing this challenge.
“It’s a very strong practice where we have intensive case managers whose entire role it is to outreach proactively to veterans who are discharging from service to try to get them engaged in the VA or to case manage them if they’re not eligible for VA to get them to the care that they can access in the community,” Dr. Semiatin said.
Helping veterans in crisis
Not every veteran is going to proactively seek help. The needs of some are only going to be discovered when they are in crisis. That’s where people like Seth Gahr, and his supervisor, Russell Conte, of the state police come in.
Conte retired as a major after 33 years with the state police. Now, as the state police mental health and wellness coordinator, he leads the state’s Crisis Intervention Training (CIT) program for first responders. He is also a longtime board member of NAMI-NH and chairs the state’s Suicide Prevention Council.
“About a third of state police are veterans,” Conte said. “And we also have a very high veteran population in New Hampshire. There’s a lot of people who served who may not be taking advantage of VA services. They may be homeless or have a substance misuse disorder or a mental health issue. When you have somebody that is either deemed suspicious or they may be homeless, whatever the case may be, many times their first interaction is not with somebody from mental health services. It’s usually the police.”
Veterans in New Hampshire
Veteran population: 93,957 (8.6% of the adult population) – 17th highest in the United States
Vietnam War veterans: 35,982 (38.3% of veterans) – 11th highest in the United States
Veterans with a disability: 25,280 (27.5% of veterans) – 12th lowest in the United States
Veteran labor force participation rate: 81% – 11th highest in the United States
Veterans living in poverty: 3.7% – the lowest in the United States
Estimated number of homeless veterans: 143
― Numbers are based on the U.S. Census Bureau’s 2018 1-year American Community Survey and the U.S. Department of Housing and Urban Development’s annual report to congress on homelessness in the United States.
What can Crisis Intervention Training help within New Hampshire
Conte said first responders who have received Crisis Intervention Training, more than 450 to date, are able to de-escalate situations. Instead of arresting someone or putting them in protective custody, they determine whether they are a veteran and, if they are, connect them with mental health services and other benefits.
Conte and others interviewed for this story urge anyone coming in contact with someone struggling with mental health to “Ask the Question,” referring to a program that trains first responders to ask “Have you or a family member ever served in the military?” to ensure veterans are identified and given the care they need.
“Prior to CIT training, there wasn’t a great referral system from law enforcement to community mental health services, including VA service,” Conte said. “So through CIT, not only do we train these people what to look for and how to identify it but who to call to get help.”
Conte said CIT trained first responders have made 1,400 contacts and referrals since the grant-funded program began three years ago. It has been so successful it just received federal funding for an additional five years.
“I’ve never met a first responder that didn’t want to help people," Conte said. "Well, if you want to help people you’ve got to do it right now. Because as soon as you drive away, if you don’t interact with that person and you don’t get them help, it’s not going to get better.”
The goal for all those who care about veterans is not simply to reduce the alarming rates of suicide, but to help veterans and their families enjoy life to the best of their abilities.

“Everyone who signs up to serve our nation is writing a blank check to the U.S. government up to and including their lives,” said Stearns of NAMI-NH. “In New Hampshire, we have a higher population of veterans than most other states and we also have a slimmer VA medical system here in NH, which really calls upon us to do things the NH way and come together as a community … to ensure that our veteran service members and their families have access to all the services and health care they require to survive and thrive.”
“I want to make sure that we frame this in terms of hope,” Stearns said. “The reality is the veterans crisis line fields about 300 calls a day. So that’s 300 folks who are reaching out for support on any given day. ... We need to remember that there are resources like the Veterans Crisis Line available. Call 988. Push 1. You’ll be connected with a veteran who can help."
Read more in this series on mental health in New Hampshire
This article originally appeared on Portsmouth Herald: NH veterans' mental health: What's the struggle and where there is help

