If you're one of 1.4M Missourians on Medicaid, confirm your contact info before April 1
For the last three years, 1.4 million Missourians on Medicaid haven't needed to re-enroll in the program yearly. That's set to change on March 31.
What is happening?
At the beginning of the COVID-19 pandemic, the US Department of Health and Human Services declared a federal public health emergency. Among other things, the declaration gave states extra Medicaid funding if they kept people continuously enrolled until the month the PHE ends. While the PHE's end date is May 11, 2023, legislation enacted in December will end the continuous enrollment requirement on March 31.
More:Despite bipartisan support, expansion of Medicaid for MO mothers could still fall short
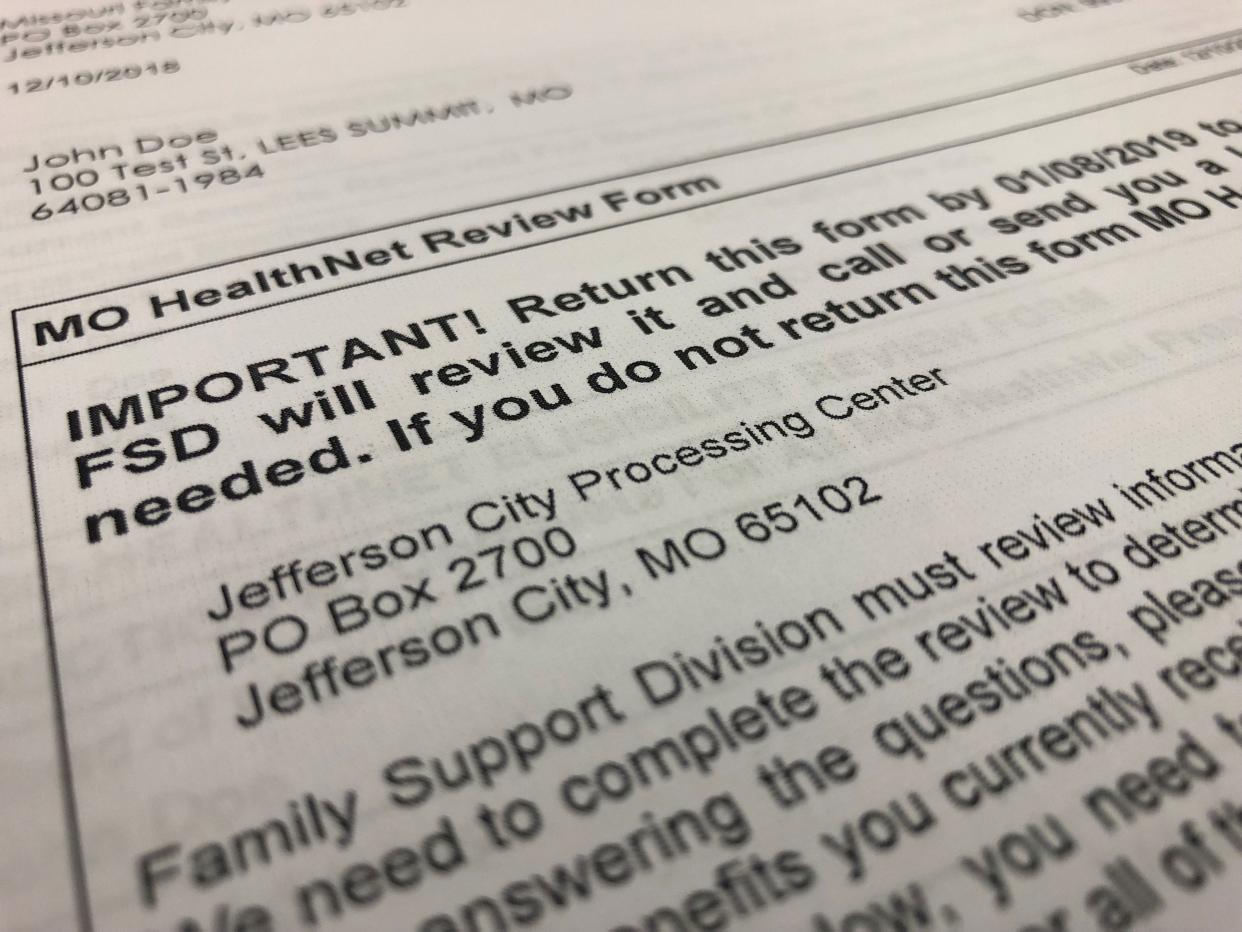
For MO HealthNet participants, including managed care health plan members, the Department of Social Services' Family Services Division will begin checking their eligibility on April 1. Participants should get a letter with what they need to do, if anything, between before April 2024, according to the DSS website.
How do I know when I'll get my letter?
Not everyone will get their letter at the same time. Given the "massive volume" of people, FSD will work a month at a time, starting with those who are due for a June 2023 annual renewal, according to Kim Evans, FSD director.
If you've been on Medicaid since before the pandemic, your annual renewal date will not change. Those who enrolled during the COVID-19 pandemic can "kind of judge (their renewal date) by the month they were approved" for Medicaid, Evans said. The DSS website has an annual renewal timeline, which tells people when they should expect a letter from FSD.
I'm on Medicaid, but didn't get a letter. What happened?
If you know your annual renewal date and haven't received a letter by the date listed on the annual renewal timeline, you should make sure FSD has your current contact information, said Becky Whiteford, outreach program manager for the Missouri Primary Care Association.
If your address has changed in the last three years, you can update that information online, at a resource center or by calling 855-373-4636. If you're having trouble navigating those options, participants can also visit showmecoverage.org or call 417-840-6788 to get in-person assistance from the MPCA.
“(MPCA is) concerned that if addresses don’t get updated — or personal contacts, like addresses, phone numbers and email addresses — that people can potentially lose their Medicaid. That’s a big concern; we do not want people going without their health coverage,” Whiteford said.
Evans also emphasized the importance of reporting changes of address: "It’s important for us to be able to get to you, and to contact individuals."
More:The U.S. population is aging. Here's how to plan ahead, find resources for long-term care
What happens if I can't get my renewal form back to FSD in time?
If someone does lose coverage because they didn't return information to FSD, they have 90 days from the end of that month to get the form turned in. If the division gets the information needed within that time frame, it will re-open the applicant's case and determine if they're still eligible for that or another level of coverage without having to re-enroll.
"They do have 90 days if they don’t get it in by the end of that month, so there is an opportunity for them to get their coverage back without having to re-apply (to Medicaid.) If they come in on day 91, they have to re-apply," Evans said.
What happens if I'm no longer eligible for Medicaid? Will I wake up without coverage?
While the exact number of people who will lose MO HealthNet coverage is currently unknown, Evans said estimates have been anywhere from 200 thousand to 300 thousand people, "but we don't know that yet." However, losing coverage shouldn't be instantaneous.
“I don’t want folks to get scared that they’re going to wake up one morning and they won’t have coverage. We will try to reach them and notify them of actions that we’re taking,” Evans said, underscoring the importance of making sure the division has current contact information.
Those who are no longer eligible, due to income or other factors, will be referred to the HealthCare.gov, the federal marketplace. Whiteford also encouraged people, if employed, to look into employer-sponsored health care.
Susan Szuch is the health and public policy reporter for the Springfield News-Leader. Follow her on Twitter @szuchsm. Story idea? Email her at sszuch@gannett.com.
This article originally appeared on Springfield News-Leader: Here's what to know before MO HealthNet annual enrollment returns

