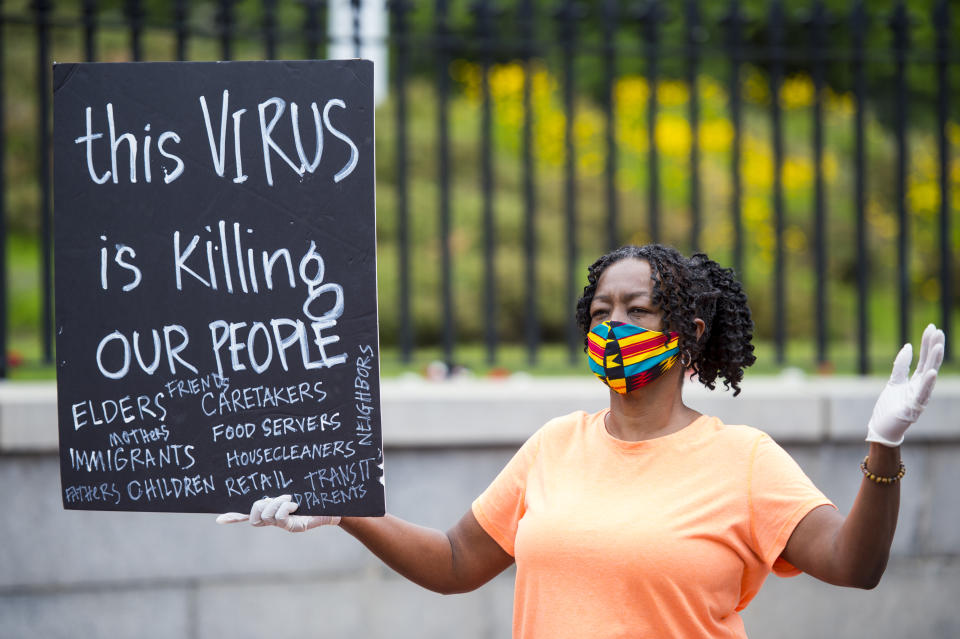
CDC: Black, Latino people make up nearly 43 percent of COVID-19 deaths
A new report from the Centers for Disease Control and Prevention Friday provides further evidence that COVID-19 is disproportionately killing Black people and Latino people, as well as other people of color. The paper, published in the CDC’s Mortality and Morbidity Weekly Report, is a follow-up to an earlier report analyzing COVID-19 deaths from Feb. 12 to May 18, which found major racial disparities among the lives lost to COVID-19.
Researchers analyzed COVID-19-linked deaths from May 1 to Aug. 31 in all 50 states and the District of Columbia, a period in which 114,411 people died. Like the earlier report, this one shows that both race and age are the two leading risk factors for death. Of the more than 114,000 who died, 78 percent were over the age of 65, 51 percent were white, 24.2 percent Latino and 18.7 percent Black. Latino people represent just 18.5 percent of the U.S. population and Black people represent 12.5 percent.
Although the percentage of deaths decreased slightly among Black people, the number of Latino deaths jumped from 16.3 percent in May to 26.4 percent in August. Asian-Americans represented 3.5 percent of overall deaths, followed by American Indian/Alaska Native individuals (although reports elsewhere show that the death rate in the latter group is much higher than for white people).
The researchers note that part of the increase in Latino deaths may be due to a shift in the regions of the U.S. where COVID-19 was spreading, but add that this does not fully explain the racial disparity. “Although there has been a geographic shift in COVID-19-associated deaths from the Northeast to the West and South, where Hispanic persons account for a higher percentage of the population, this analysis found that ethnic disparities among decedents in the West and South increased during May-August, 2020, suggesting that the geographic shift alone does not entirely account for the increase in the percentage of Hispanic decedents nationwide.”
Dr. Uché Blackstock, Advancing Health Equity CEO and Yahoo Life medical contributor, says that social determinants of health — conditions or environments in which people “live, work and play” — may explain the increase. “I definitely think for a Hispanic population you have to think about the issue of access to health care as connected to immigration status,” says Blackstock. “We know that if people are undocumented that they may not have access to health care, which could influence whether they have access to testing, or to a health care facility if they become sick.”
Other social determinants of health may influence the disparity among Latinos as well as Black people, including the fact that both groups are more likely than whites to be essential workers. The CDC elaborates: “Inequities in the social determinants of health can lead to increased risk for SARS-CoV-2 exposure among some racial and ethnic groups. For example, persons from underrepresented racial and ethnic groups might be more likely to live in multigenerational and multifamily households, reside in congregate living environments, hold jobs requiring in-person work (e.g., meatpacking, agriculture, service, and health care), have limited access to health care, or experience discrimination.”
Blackstock adds that Black people — who are twice more likely to die of COVID-19 than white people — also have higher rates of underlying conditions that put them at risk of serious illness. This can be linked to inequality too. “Even though we’re saying that social determinants are playing a part in who gets infected and dies, we also knew that before this pandemic the social determinants were key in influencing which communities carry the highest burden of chronic disease, like diabetes, obesity, asthma and hypertension,” says Blackstock. “All of the underlying medical problems that we know put people at risk for doing very poorly if they’re infected with the coronavirus.”
Overall, she says, the new data is not surprising, but that the fact that age and race were listed as the two main risk factors for death underscores the toll that racism takes on the bodies of those who endure it. “It’s almost as if living in a country with racism ages people. It ages their bodies to the point where even people who are not elderly — because they are people of color living in a country with racism — are still susceptible to dying from this virus in a way that’s very similar to people who are elderly.”
Blackstock, who has dedicated her career to fighting racial inequality in the health care world, urges the government to act when it comes to providing resources to these communities. “It’s predictable that we would see that there was no strategy to support those communities, which were vulnerable even before the pandemic,” she says. “[But] if there’s no strategy to support those communities, we’re going to continue to see increasing hospitalizations and deaths.”
For the latest coronavirus news and updates, follow along at https://news.yahoo.com/coronavirus. According to experts, people over 60 and those who are immunocompromised continue to be the most at risk. If you have questions, please reference the CDC’s and WHO’s resource guides.


