COVID-19 is on the rise again in the Mohawk Valley. What you need to know.
Got the sniffles or a cough? Could be a cold. Or the flu. Or RSV. Or COVID-19.
They’re all circulating in the Mohawk Valley right now, often wreaking respiratory havoc, although COVID-19 can present without respiratory symptoms.
There is, in fact, enough COVID-19 cases around right now for some health systems, including the Mohawk Valley Health System, to have put mask rules back in place in some local health care facilities.
That’s not to say that the numbers are as high as in past winters, although only tests performed in a lab are counted in state statistics.
In the Mohawk Valley, 55 samples tested positive for COVID-19 in labs from Dec. 30 to Jan. 5, giving the region the fewest cases per 100,000 residents of any region in the state — 11.3. Oneida County had 18 cases, or 7.8 per 100,000 residents; Herkimer County had 12 cases, or 19.4 per 100,000 residents.
Long Island, followed by the Hudson Valley, had the highest case rates in the state.
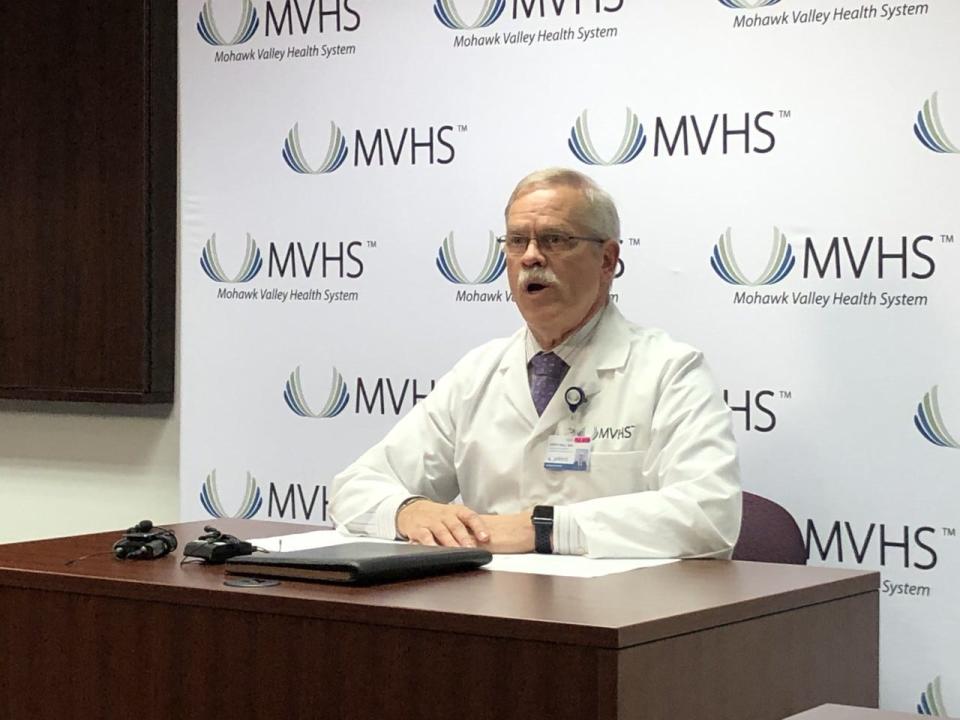
Dr. Kent Hall, chief physician executive for MVHS, who started his job a just over a month before the COVID-19 pandemic lockdown, served as the health system’s chief spokesperson during the pandemic, updating the media on the situation in the health system’s, at that time, two hospitals, and sharing public health messages about prevention.
He was even recognized in public sometimes after appearing on so many newscasts.
Hall, who is retiring at the end of the month, spoke to the O-D once more about the local COVID-19 situation. Here’s what he had to say:
What is MVHS seeing right now in terms of COVID-19 and other wintertime illnesses?
On Friday afternoon, the Wynn Hospital had 16 COVID-positive inpatients, down by almost 10 from Thursday, Hall said. The hospital recently had 33 COVID-19 patients.
Another 11 patients had been exposed to COVID-19 and were being watched to see if they developed COVID-19. The hospital also had six patients with the flu and one with RSV, a decrease from a few days ago.
RSV is cyclical and Hall said he expects that number to rise again by Monday.
Why did MVHS decide to mandate masks again for patients, visitors and staff in most situations within its facilities, including the Wynn Hospital?
MVHS had set its own internal parameters for when it would require masks in some or all of its facilities. One criteria was set as clusters of outbreaks among staff in three or more departments in the hospital, medical practices or administrative offices outside the hospital.
MVHS saw four clusters on inpatient units as well as clusters at three different practices.
“These are not clusters that were caused by people being exposed to people in the hospital,” Hall said. “These are actually things that people brought in.”
The health system also had a threshold for the number of patients hospitalized with COVID-19, which it has not met. But the hospital did see a rapid, significant increase in the number of patients with COVID-19, Hall said.
Visitors are included in the mask mandate because the rate of transmission in the community has gone up, likely because the dominant variant now, JN.1, is more easily transmissible, he said. Officials don’t want to see visitors transmit COVID-19 to patients who are already sick.
Is COVID-19 making patients as sick as it used to?
In general, no. Most patients are not getting as sick as they did back in the winter of 2021. During the last three or four weeks, only two COVID-19 patients at MVHS ended up in the intensive care unit, far fewer than in 2021.
Hall said he thinks there are two reasons that fewer people are getting so sick with COVID-19. “Almost everybody who is around has had some degree of exposure and, therefore, developed some kind of immunity,” he said, “whether it’s natural immunity because they’ve had the disease or they’ve had the vaccine or both.”
And, as new variants come along, the severity of the disease seems to decline although, at the same time, it becomes easier to spread. Hall suspects, he said, that it will eventually (and he could not speculate on a timeframe) become less severe, possibly like the flu or at least, a bad case of the flu.
How does this year’s flu season look?
It started four or five weeks later than last year’s and hasn’t peaked yet, but looks like it will be about the same or almost the same as last year’s flu season.
“Last year’s flu season was very bad,” Hall said. “it caused a lot of people in the community to be sick and it caused a lot of hospitalizations, more so than in prior years.”
More: 15-year-old Utica resident shot and killed, police say
More: Oneida Indian Nation opens Verona Collective dispensary. See photos from the grand opening
Flu shots are the best defense against the flu, but public health officials won’t know how effective this year’s shot is until the end of flu season.
What are COVID-19 symptoms to look for in 2024?
Nasal congestion, a sore throat, aches and pains, a cough (most often, one that’s non-productive), a headache, nausea and vomiting, and a fever can all be symptoms of COVID-19, among other things. The loss of smell or taste is a possible COVID symptom, too.
More severe symptoms include shortness of breath and a prolonged, high fever.
Another specific COVID-19 symptom is a higher level of fatigue.
“They just get tired,” Hall said, “to the point where, even with mild upper respiratory symptoms — oh my gosh, do I even have the strength to get out of bed? Thankfully, that’s not hugely common.”
What to do if you have symptoms?
If they’re mild enough not to require medical attention, stay home, take care of yourself and stay away from others, especially those who may be more at risk for more severe illness.
When should you take an at-home COVID-19 test?
If you have any symptoms and will be around other people, particularly if you’re going to be around people for any length of time — dinner out, a movie, work — take a test and don’t go if it’s positive.
If it’s negative and you decide to go, consider wearing a mask so you don’t spread other germs.
If you have COVID-19, how long do you need to stay away from other people?
National and state guidelines say that anyone testing positive should isolate for at least five days. If after five days you no longer have active symptoms —things like a high fever, shortness of breath, a severe cough — then you are no longer infectious and can stop isolating.
If you still have active symptoms, continue to isolate for another five days. After 10 days, you should be better and if not, you should see a doctor because you might have a health issue besides COVID-19.
Some people continue to test positive for COVID-19 for a few months because the test can detect remnants of the virus, even when the person is no longer infectious, so a negative test is not a requirement to end isolation.
Some workplaces may have different requirements for isolation, so make sure you know your employer’s policy.
When should you wear a mask?
If you’re not feeling well and are going to be with people in an enclosed environment for an extended period of time, it’s a good idea to mask, even if you’ve taken a COVID-19 test and it was negative.
Some people are more comfortable masking all of the time and that’s fine, too. Masking protects other people, who may be more vulnerable to severe illness, but it also protects the person wearing the mask.
People with health problems, such as emphysema or other respiratory issues, heart problems, diabetes, autoimmune diseases, cancer or being overweight, are at higher risk and could consider masking as a precaution.
Were you originally hired to keep track of COVID-19?
Absolutely not.
When he started in Feb. 2020, Hall expected to concentrate on helping the health system prepare for the move into the Wynn Hospital (which happened in October), working to unify the culture of the medical staffs at the two hospitals that then existed and starting new graduate medical education programs (a number of which have begun).
What will you do in retirement?
Hall wants to spend more time on non-medical pursuits, he said, such as visiting his 12 grandchildren and working on his landscape photography hobby.
This article originally appeared on Observer-Dispatch: COVID-19 cases, quarantines, masking in Mohawk Valley now

